Presenter: Robert J. Zabel, DO
Dermatology Program: Philadelphia College of Osteopathic Medicine / Lehigh Valley Hospital
Program Director: Stephen Purcell, DO
Submitted on: Aug 29, 2002
CHIEF COMPLAINT: Chest pain and shortness of breath
CLINICAL HISTORY: A 60-year-old Hispanic female with a two-year history of idiopathic crescentic glomerulonephritis presented with chest pain and shortness of breath. Cardiac ischemia was excluded from serial lab studies and intravenous heparin was started for a potential pulmonary embolism. On hospital day three, subcutaneous nodules were noted on her forehead. These nodules rapidly increased in size and number over a 24-48 hour period. They spread rapidly over the face, neck, upper trunk, and upper extremities. The subcutaneous nodules transitioned to exophytic and weeping lesions. On hospital day seven, she developed a productive cough with blood-tinged sputum and a chest radiograph showed diffuse bilateral infiltrates. A pulmonary angiogram was negative for an embolism and anticoagulation was stopped. A bronchoscopy revealed nodules lining the bronchi and diffuse alveolar hemorrhage.
PHYSICAL EXAM:
Subcutaneous nodules becoming exophytic and weeping with crust over the face, neck, upper trunk, and upper extremities. There was a 2cm. hemorrhagic bullous lesion on the left palm. A few oral mucosal ulcers were present.


LABORATORY TESTS:
PAS, Gram’s stain, Fite stain, and cultures were all negative. Leukocytosis with a normal eosinophil count. ESR and CRP elevated. Positive P-ANCA and C-ANCA
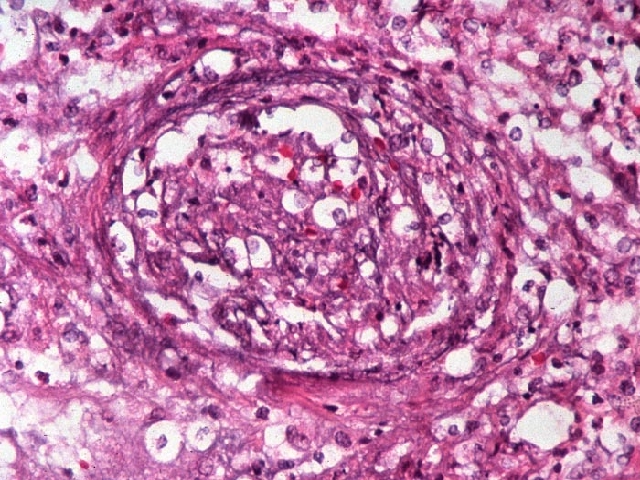
DERMATOHISTOPATHOLOGY:
Microscopic description: Biopsies showed a large amount of tissue edema, full-thickness necrosis of a medium-sized arteriole, neutrophilic infiltrate, and karyorrhexis.
DIFFERENTIAL DIAGNOSIS:
1. Churg-Strauss Syndrome
2. Lymphomatoid Granulomatosis
3. Wegener’s Granulomatosis
4. Temporal Arteritis




