CORRECT DIAGNOSIS:
Cryptococcus neoformans
DISCUSSION:
Cryptococcus neoformans is an encapsulated yeast like fungus. Strains are grouped into two varieties that include five serotypes known as C. neoformans variety neoformans (serotypes A, D, and AD) and C. neoformans variety gattii (serotypes B and C). The serotype differences reflect antigenic differences in the structure of the capsular polysaccharide. C. neoformans var. neoformans is found throughout the world in association with excreta from certain birds including pigeons, chickens, canaries, and cockatoos. C. neoformans var. gattii is found primarily in tropical and subtropical regions and has been associated with several species of eucalyptus trees.
In order to cause disease in humans, the fungus must be inhaled into the lungs, although a small percentage of patients can develop primary cutaneous cryptococcus after direct implantation. Once within the lungs, C. neoformans can cause a variety of symptoms from asymptomatic colonization to severe pneumonia. From the lungs, the organisms disseminate to the blood and subsequently any organ system. The CNS is the most common site of dissemination.
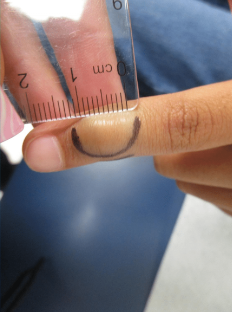
The skin is the second most common site of cryptococcal dissemination, occurs in 10-20% of patients, and is often the presenting sign of disease. Cutaneous manifestations of disseminated disease are protean and most commonly occur on the head and neck. Although molluscum-like lesions are the most common, acneiform lesions, purpura, vesicles, tumors, abscesses, oral and genital ulcers, granulomas, plaques, sinus tracts, cellulitis, subcutaenous nodules, and HSV-like lesions have all been reported. Direct cutaneous cryptococcosis caused by direct trauma is rare and produces solitary nodules that ultimately break down or ulcerate. Lymphadenopathy may or not be present. Biopsy specimens will often show two types of histological patterns: gelatinous and granulomatous. This patient’s biopsy consisted of the gelatinous type, which produces little inflammatory reaction and numerous organisms (4 to 12 mum) with large polysaccharide capsules. The capsule stains purple with methylene blue, blue with alcian blue, and red with mucicarmine. The granulomatous type produces more of an inflammatory reaction with giant cells and a small number of organisms. The organisms are 2 to 4 mum, have thin or no capsules, and are found within giant or mononuclear cells. The fungi stain red with PAS, black with methanamine silver, and dark brown with Fontana-Masson.
TREATMENT:
Once disseminated cryptococcosis has been ascertained, the treatment approach relies heavily on amphotericin B (0.7-1 mg/kg/d) plus flucytosine (100 mg/kg/d for 2 weeks) followed by fluconazole (400 mg/d) for a minimum of 10 weeks in the immunocompromised host. Amphotericin was used to treat this patient.
Ambisone at 4 mg/kg/day has been shown to perform similar to Amphotericin B. Fluconazole (400-800 mg/d) plus flucytosine (100-150 mg/kg/ d) for 6 weeks is an alternative to the use of amphotericin B, although toxicity with this regimen is high. For those patients with HIV who present with isolated pulmonary or urinary tract disease, fluconazole (200-400 mg/d) is indicated and itraconazole (200-400 mg/d) is an acceptable alternative.
REFERENCES:
Schupbach, D. W., Wheeler, C. E., Briggaman, R. A., et al. (1976). Cutaneous manifestations of disseminated Cryptococcus. Archives of Dermatology, 112(12), 1734–1740. https://doi.org/10.1001/archderm.1976.03850090042010 [PMID: 187642]
Perfect, J. R. (1989). Cryptococcosis. Infectious Diseases Clinics of North America, 3(1), 77–102. https://doi.org/10.1016/S0891-5520(18)30057-3 [PMID: 2642582]
Dimino-Emme, L. (1995). Cutaneous manifestations of disseminated Cryptococcus. Journal of the American Academy of Dermatology, 32(5 Pt 2), 844–850. https://doi.org/10.1016/S0190-9622(95)90071-3 [PMID: 7757886]
Bennett, J. E., Dismukes, W., Duma, R. J., Medoff, G., Sande, M. A., Gallis, H., et al. (1979). A comparison of amphotericin B alone and combined with flucytosine in the treatment of cryptococcal meningitis. New England Journal of Medicine, 301(3), 126–131. https://doi.org/10.1056/NEJM197907193010301 [PMID: 45186]
Lever, W. F., & Schaumberg-Lever, G. (1990). Histopathology of the skin. Philadelphia: J.B. Lippincott. p. 379–381.