CORRECT DIAGNOSIS:
Oral Lichen Planus
DISCUSSION:
Oral lichen planus (OLP) can be a very frustrating disease for both the patient and the dermatologist. Patients with symptomatic OLP often require intensive therapy to reduce the signs and symptoms of this painful and disabling inflammatory disease. Although controversial, patients with OLP may develop oral squamous cell carcinomas (OSCC). This patient subsequently developed OSCC five years after developing OLP.
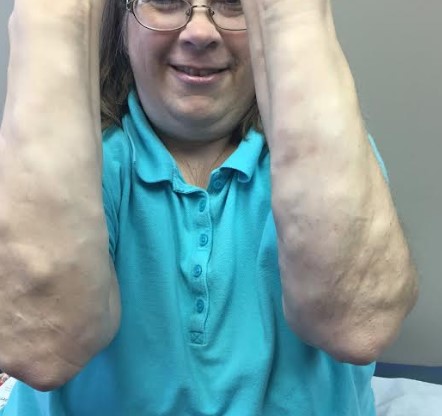
While the pathogenesis of OLP is complex and not completely understood, extensive painful erosions can lead to a significant decrease in quality of life. OLP tends to be an unremitting disease, with reticulate (1/3 of cases), atrophic (1/5 of cases), and ulcerative forms. This patient demonstrates all three variants of OLP, as well as “vulvovaginal-gingival syndrome”, a distinct subset with concomitant genital involvement. Since many patients with OLP have “extra-oral” manifestations, a multidisciplinary medical team should routinely perform a thorough history and physical examination.
TREATMENT:
The principal aims of OLP therapy were the resolution of oral mucosal lesions and painful symptoms, as well as the maintenance of good oral hygiene. Topical corticosteroids, antimycotics, and calcineurin inhibitors have been the mainstay of treatment. Other measures include routine clinical examinations and the elimination of smoking and alcohol to reduce the risk of OSCC.
Given the age and health of the patient, more aggressive modalities were not viable. Currently, there is no curative treatment available for OLP; however, immunomodulation may provide potential benefits. OLP that is recalcitrant to topical corticosteroids may respond to topical tacrolimus. Other potential therapies for recalcitrant OLP include mycophenolate, systemic corticosteroids, retinoids, hydroxychloroquine, azathioprine, and dapsone.
REFERENCES:
Dissemond, J. (2004). Oral lichen planus: An overview. Journal of Dermatological Treatment, 15(3), 136-140. https://doi.org/10.1080/09546630410012989
Eisen, D. (2002). The clinical features, malignant potential, and systemic associations of oral lichen planus: A study of 723 patients. Journal of the American Academy of Dermatology, 46(2), 207-214. https://doi.org/10.1067/mjd.2002.120092 [PMID: 11898044]
Eisen, D. (1994). The vulvovaginal-gingival syndrome of lichen planus: The clinical characteristics of 22 patients. Archives of Dermatology, 130(11), 1379-1382. https://doi.org/10.1001/archderm.130.11.1379 [PMID: 7962450]
Eisen, D. (1999). The evaluation of cutaneous, genital, scalp, nail, esophageal, and ocular involvement in patients with oral lichen planus. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 88(4), 431-436. https://doi.org/10.1016/S1079-2104(99)70047-0 [PMID: 10572149]
Itin, P., Surber, C., & Buchner, S. (1992). Lack of effect after local treatment with a new cyclosporin formulation in recalcitrant erosive oral lichen planus. Dermatology, 185(4), 262-265. https://doi.org/10.1159/000246564 [PMID: 1466421]