Presenter: David B. Roy D.O.
Dermatology Program: Midwestern University of Health Sciences
Program Director: Don A. Anderson D.O.
Submitted on: July 30, 2006
CHIEF COMPLAINT: Sudden onset of dyspnea and cough with hemoptysis as well as a painful rash on face and legs
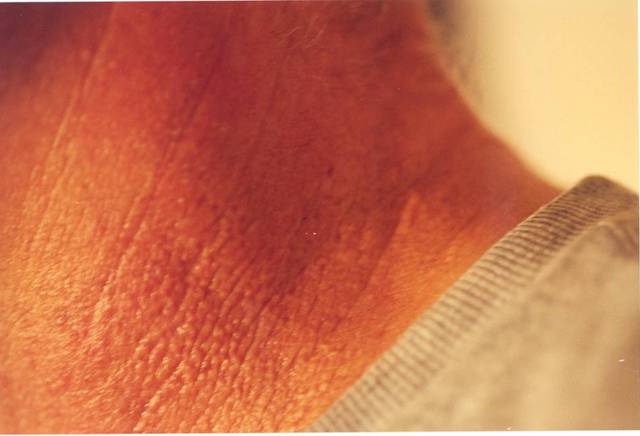
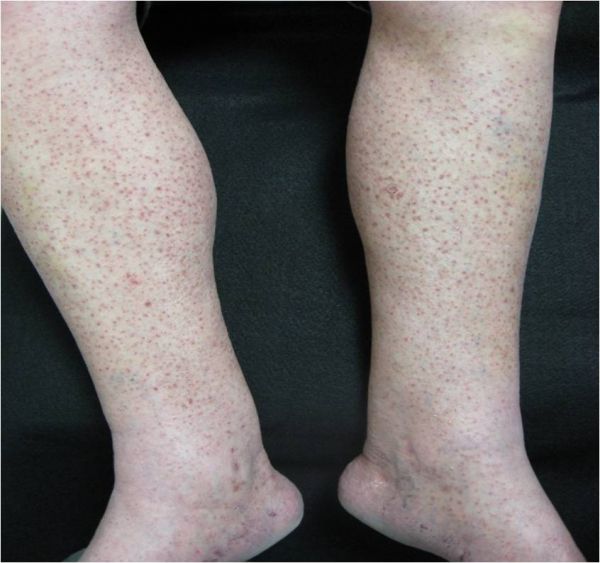
CLINICAL HISTORY: A 70-year-old white male with MI, tobacco use, hypertension, coronary artery disease, and a sedentary lifestyle presented to clinic complaining of a sudden onset of dyspnea and cough with hemoptysis as well as a painful rash on face, legs, perinasal area, and perioral area with ulceration. Patient also endorses congestion, hematuria, difficulty walking, and weakness. The patient had completed a course of PO prednisone approximately two months earlier due to an unspecified rash of the lower extremities.
PHYSICAL EXAM:
Temp – 98˚F
BP – 90/30 arterial line
HR – Low 100’s sinus tach
RR – 20
O2 Sat – 96% non rebreather
Examination of the skin revealed palpable purpura of the bilateral lower extremities. There were several erythematous nodules with shallow ulcerations of the perinasal/oral areas.



LABORATORY TESTS:
H/H – 8.4/28
WBC – 8
U/A – positive for RBC’s, protein, sediment
BUN – 50
Creat – 2.2
CXR – CHF with patchy infiltrates
ESR and CRP – elevated
C-ANCA – positive
DERMATOHISTOPATHOLOGY:
Non-specific perivascular inflammation of small arteries and veins with necrosis and fibrin deposition of vessel walls, red blood cell extravasation, thrombi, and nuclear dust. Granulomatous inflammation in the blood vessels and surrounding dermis was also noted. No atypical lymphocytes noted.
DIFFERENTIAL DIAGNOSIS:
1. Wegener’s Granulomatosis
2. PAN
3. Lymphomatoid Granulomatosis
4. Churg-Strauss
5. SLE