CORRECT DIAGNOSIS:
Paraneoplastic dermatitis
DISCUSSION:
There are several case reports linking ichthyosis as a paraneoplastic skin finding to hematological malignancies. Although paraneoplastic ichthyosis is generally associated with hematological malignancies, it has also been associated with solid tumors as well. In a small case study published in early 2012 from France, five patients were diagnosed with hematological malignancies that developed ichthyotic skin findings shortly after. Four of the five cases had partial or complete resolution of skin findings with the treatment of their underlying disease. Because of this, the authors believe paraneoplastic ichthyosis is a reliable treatment monitoring tool. A similar case report revealed the resolution of ichthyotic skin after adenectomy for the treatment of large-cell anaplastic lymphoma.
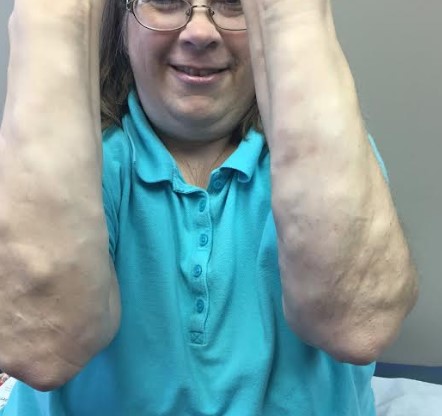
Our patient’s clinical presentation was highly suspicious for acquired ichthyosis. Our index of suspicion was high because of his elevated eosinophils and clinical findings so we opted to refer him to hematology/oncology for a full workup. He was found to have non-Hodgkin’s lymphoma. Acquired ichthyosis is a rare finding in patients with non-Hodgkin’s lymphoma. Although our patient’s pathology did not reveal the expected hypogranulosis and compact hyperkeratosis expected in acquired ichthyosis, we still believe his dermatitis was an indication of systemic disease.
Occasionally internal malignancies can manifest as cutaneous findings. We present a case of a seventy-four-year-old male with an eighteen-week history of recalcitrant dry and itchy skin. He had concomitant sixteen-pound weight loss, change of taste, and one month of intermittent diarrhea. On physical exam, he had diffuse ichthyotic integument with sparing of the folds. Despite pathological findings being inconsistent with the clinical picture, he was referred to hematology/oncology and subsequently diagnosed with non-Hodgkin’s lymphoma. Dermatologists and other physicians need to keep a high index of suspicion to diagnose some paraneoplastic syndromes. If treatment is not satisfactory or clinical presentation does not correlate with pathological or another testing, further evaluation is necessary. Treatment of the underlying malignancy has shown to improve, if not resolve, the paraneoplastic cutaneous findings.
We were unable to monitor the patient’s cutaneous findings because he chose not to undergo treatment of his malignancy and has since passed.
TREATMENT:
Triamcinolone 0.1% cream, UVB therapy 3x weekly, hydroxyzine 25mg nightly
REFERENCES:
Ann Dermatol Venereol. 2012 Jan;139(1):9-14. Epub 2011 Dec 3
Ann Dermatol Venereol. 2001 Jan;128(1):31-4.
Intern Med. 2007;46(7):397-9. Epub 2007 Apr 2.
J Am Acad Dermatol. 2009 Sep;61(3):538-40
Isr Med Assoc J. 2009 Feb;11(2):121-2