Presenter: Hamblin, T., DO; Brindise, R., DO; Laffer, M., OMS-IV; Grekin, S., DO
Dermatology Program: Oakwood Southshore Medical Center
Program Director: Steven Grekin, DO
Submitted on: April 6, 2013
CHIEF COMPLAINT: Pruritic “sun spots” on both lower extremities
CLINICAL HISTORY: A 33-year-old Caucasian woman noticed in 1999 the appearance of pruritic “sun spots” on both lower extremities. She associated the appearance of the lesions with taking antibiotics that she received for strep pharyngitis. She did not remember the name of the antibiotics but did recall that the packaging specified the need for sun avoidance while taking them. She was, however, exposed to several hours of sun each day while vacationing during this time, and noticed the development of the lesions within one week of being on the medication. She subsequently presented to our clinic in June of 2007. She notes that she consulted dermatology out of curiosity regarding the lesions as well as for guidance regarding the severe pruritus associated with them. She noted that the pruritus was much worse with activity and in the winter season, but improved when the involved areas were exposed to sunlight. Review of systems was negative for flushing, lightheadedness, dizziness, anaphylaxis, nausea, vomiting, diarrhea, and bone or muscle pain. The patient’s medical history was unremarkable. Family history was negative for any chronic cutaneous disorders or other related findings.
Previous Treatment: Prior to the availability of the biopsy, the patient was prescribed salicylic acid cream to apply to the affected areas at bedtime. On post-biopsy follow-up, it was advised that the patient begins NB UVB therapy and begin daily supplementation with Vitamin C. The patient did not pursue NB UVB therapy as this was not feasible for her with her schedule. She did not return until 2010 for follow-up, during which time NB UVB therapy was again recommended, along with supplementation with daily Vitamin D. She declined NB UVB once again. She returned in 2011 for an unrelated lesion and follow-up her lower extremity lesions. It was noted at this time that lesions were now present on bilateral upper extremities as well. She was prescribed a mid-potency topical steroid. She was not seen again until recently in 2012, when it was noted that the lesions were now also involving the trunk, but sparing the face. She noted that she has been taking both Vitamin C and D inconsistently over the last several years. She also noted that she occasionally takes OTC cetirizine and diphenhydramine when the pruritus becomes intolerable, particularly in the winter time. She noted that the sun significantly decreases the pruritus during the summer months and decreases her requirement for anti-histamines.
PHYSICAL EXAM:
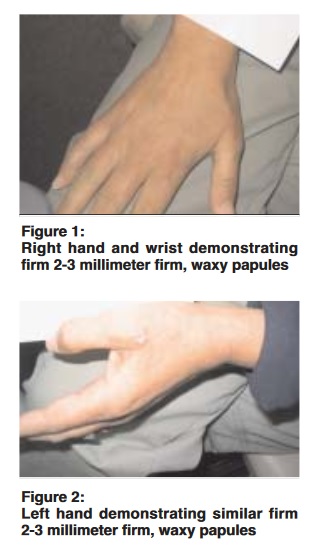
On the first examination, it was noted that the patient had red-brown to violaceous papules scattered over her bilateral lower extremities, most heavily localized on her anterior, upper thighs.

LABORATORY TESTS: N/A
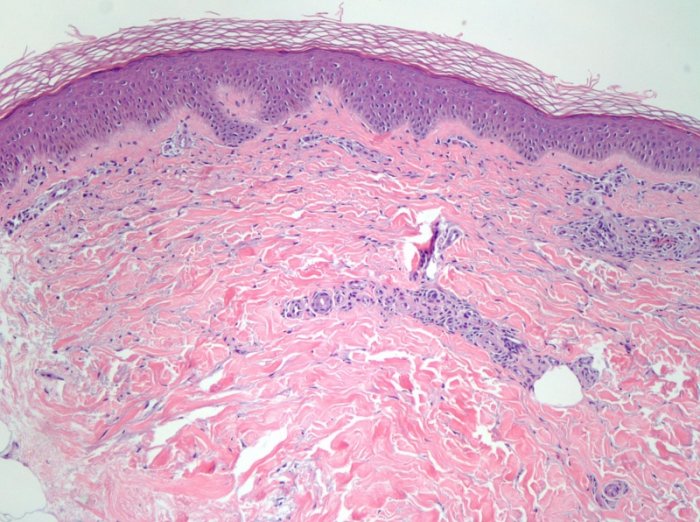
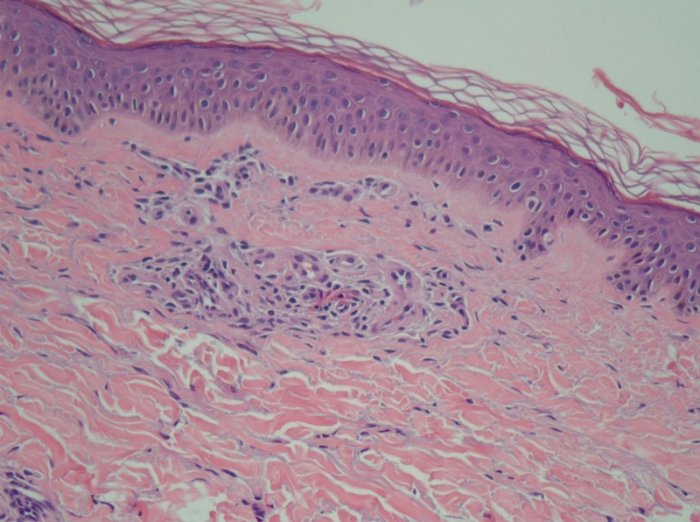
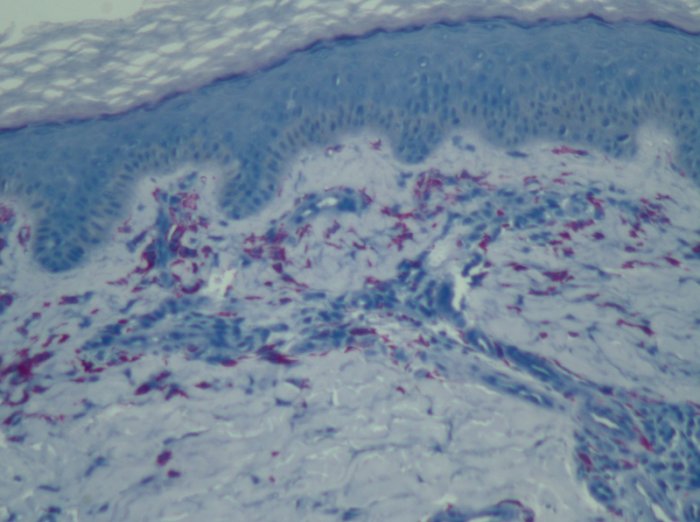
DERMATOHISTOPATHOLOGY:
Punch biopsy in 2007 obtained from her right upper thigh revealed a sparse infiltrate made up predominantly of mast cells present around prominent dilated vessels of the superficial vascular plexus, highlighted by a Leder stain.
DIFFERENTIAL DIAGNOSIS:
1. Lichen planus
2. Cholinergic urticaria
3. Telangiectasia macularis eruptiva perstans
4. Diffuse cutaneous mastocytosis
5. Poikiloderma vasculare atrophicans