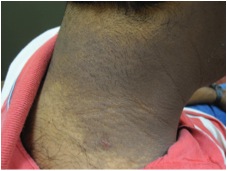
CORRECT DIAGNOSIS:
Atypical vascular lesion
DISCUSSION:
Over the past decade, a direct link has been established between the development of angiosarcoma and radiation treatment, specifically on the breast. Although the relative risk is about 10-fold, the overall incidence of angiosarcoma arising in a breast radiation field falls within an estimated range of 0.09 to 0.16%. The specific inciting requirements are speculated to be a result of breast-conserving surgery, chemotherapy, and post lumpectomy radiation treatment. Interestingly, atypical, but not outwardly malignant vascular lesions have been reported to develop in radiation fields following breast-conserving surgery as well. Clinical and histologic overlap, combined with an unpredictable long term clinical course, may cause difficulty in distinguishing atypical vascular lesions (AVLs) from early angiosarcoma. An established treatment protocol is needed for patients that fall into this category.
AVLs typically present in women in their 50s that have received breast-conserving surgery, in conjunction with an average treatment of 40-60 Gy cumulative radiation dose. Clinically, these lesions tend to be smaller, well-circumscribed, and symmetrical. The post-radiation interval for the development of AVLs is notably shorter compared to frank angiosarcoma. The time to presentation for AVLs is approximately 3 years compared to angiosarcoma, which is approximately 6yrs. This has led to the hypothesis that AVLs and angiosarcoma are part of a continuous spectrum of vascular lesions, and that AVLs represent a precursor lesion.
Histopathologic analysis of AVLs versus angiosarcoma can be difficult due to many different overlapping features. To date, angiosarcoma has been histopathologically identified by anastomosing vascular channels lined by prominent endothelial cells with nuclear hyperchromasia and hobnailing. Dissection of dermal collagen and involvement of the subcutaneous tissue can occur in conjunction with necrosis or “blood lakes”. AVLs, in contrast, appear well-circumscribed, wedge-shaped, and tend to involve only the superficial to mid dermis. Recently, fluorescence in situ hybridization (FISH) has been able to distinguish AVLs from angiosarcoma by the presence of MYC amplification, although repeat testing on multiple biopsy sites may be needed for consistent results.
No definitive criteria are available to adequately predict whether AVLs will develop into angiosarcoma or may continue to follow a benign course. Recent attempts at sub-classifying lesions with similar histopathologic findings into two categories (i.e. lymphatic appearing versus capillary appearing lesions) have not been found to be a definitive means of distinguishing AVLs of a more aggressive nature, or those that may develop into angiosarcoma. Analysis of new cases with long term follow-up is needed to further analyze the spectrum of these lesions, leading to an appropriate and accepted treatment algorithm in the future.
TREATMENT:
Serial breast exams in conjunction with routine mammography. Biopsy of any new or changing lesions.
REFERENCES:
Brenn, T., & Fletcher, C. D. (2005). Radiation-associated cutaneous atypical vascular lesions and angiosarcoma: clinicopathologic analysis of 42 cases. Am J Surg Pathol, 29(8), 983-996. PMID: 15951895
Brenn, T., & Fletcher, C. D. (2006). Postradiation vascular proliferations: an increasing problem. Histopathology, 48(2), 106-114. PMID: 16433731
Patton, K. T., Deyrup, A. T., & Weiss, S. W. (2008). Atypical vascular lesions after surgery and radiation of the breast: a clinicopathologic study of 32 cases analyzing histologic heterogeneity and association with angiosarcoma. Am J Pathol, 172(3), 943-950. PMID: 18285530
Fernandez, A., Sun, Y., Tubbs, R. R., Goldblum, J. R., & Billings, S. D. (2012). FISH for MYC amplification and anti-MYC immunohistochemistry: useful diagnostic tools in the assessment of secondary angiosarcoma and atypical vascular lesion proliferations. J Cutan Pathol, 39(3), 234-242. PMID: 22171818