CORRECT DIAGNOSIS:
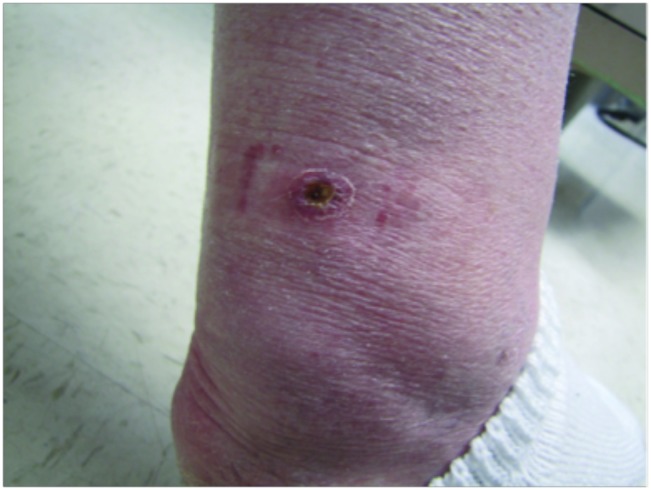
Sebaceous adenoma consistent with Muir Torre Syndrome
DISCUSSION:
Muir Torre Syndrome is a rare, autosomal dominant genodermatosis more commonly seen in males with a mean age of first cutaneous manifestation at 55 years. This disease is characterized by sebaceous neoplasms, keratoacanthomas, and visceral malignancy. Muir Torre represents a sub-type of Hereditary Non-polyposis Colorectal Cancer or Lynch Syndrome.
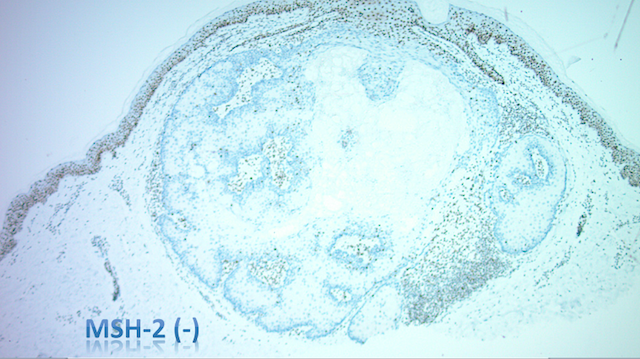
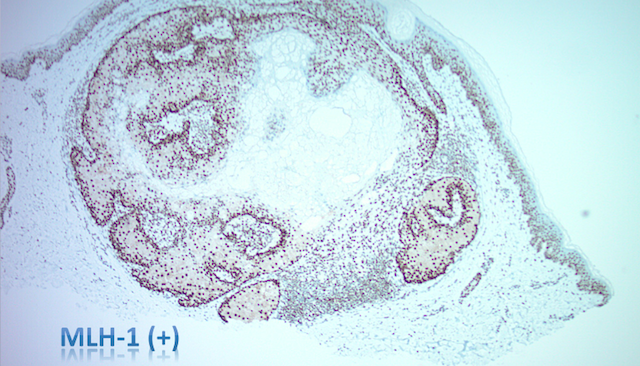
Muir Torre syndrome is caused by heterozygous germline mutations in one of several DNA mismatch repair genes, including MSH2 (approximately 90% of MTS cases), MLH1, and MSH6. The somatic loss of heterozygosity occurs due to the inactivation of the other allele of the affected gene. This results in microsatellite instability and tumor formation.
Clinically, cutaneous neoplasms may present decades prior to visceral malignancy. Sebaceous neoplasms tend to favor head/neck, but when observed outside this region, they are highly suggestive of Muir Torre Syndrome. Sebaceous adenomas are the most common neoplasm and keratoacanthomas are observed in 25% of patients.
Gastrointestinal malignancy is seen in 61% of patients, most commonly found in the proximal colon with average age onset of 50 years old. Other associated malignancies include genitourinary (22%), hematologic malignancies (11%), breast carcinomas (6%), head and neck cancers (5%), and neoplasms of the small intestine (3%). Diagnosis requires 1 sebaceous tumor and 1 visceral tumor.
TREATMENT:
Since our patient had not yet developed internal malignancy, biennial colonoscopy, renal U/S, and CBC and UA were suggested. Given the inheritance pattern of this disease, genetic counseling is recommended.
Sebaceous adenomas may be treated with excision, ED&C, cryosurgery, or radiotherapy. Additionally, oral retinoids may be considered to prevent the development of more sebaceous neoplasms.
REFERENCES:
South, C. D., Hampel, H., Comeras, I., et al. (2008). The frequency of Muir-Torre syndrome among Lynch syndrome families. Journal of the National Cancer Institute, 100, 277–281. https://doi.org/10.1093/jnci/djn017
Mangold, E., Rahner, N., Friedrichs, N., et al. (2007). MSH6 mutation in Muir-Torre syndrome: Could this be a rare finding? British Journal of Dermatology, 156, 158–162. https://doi.org/10.1111/j.1365-2133.2006.07838.x
Lynch, H. T., & Fusaro, R. M. (1999). The Muir-Torre syndrome in kindreds with hereditary nonpolyposis colorectal cancer (Lynch syndrome): A classic obligation in preventive medicine. Journal of the American Academy of Dermatology, 41, 797–799. https://doi.org/10.1016/S0190-9622(99)70093-2
Dores, G. M., Curtis, R. E., Toro, J. R., et al. (2008). Incidence of cutaneous sebaceous carcinoma and risk of associated neoplasms: Insight into Muir-Torre syndrome. Cancer, 113, 3372–3381. https://doi.org/10.1002/cncr.24008
Eisen, D. B., & Michael, D. J. (2009a). Sebaceous lesions and their associated syndromes: Part I. Journal of the American Academy of Dermatology, 61, 549–560. https://doi.org/10.1016/j.jaad.2009.05.028
Eisen, D. B., & Michael, D. J. (2009b). Sebaceous lesions and their associated syndromes: Part II. Journal of the American Academy of Dermatology, 61, 563–578. https://doi.org/10.1016/j.jaad.2009.05.029
Curry, M. L., Eng, W., Lund, K., et al. (2004). Muir-Torre syndrome: Role of the dermatopathologist in diagnosis. American Journal of Dermatopathology, 26, 217–221. https://doi.org/10.1097/01.dad.0000134542.04618.1e
Cohen, P. R. (1992). Muir-Torre syndrome in patients with hematologic malignancies. American Journal of Hematology, 40, 64–65. https://doi.org/10.1002/ajh.2830401312