CORRECT DIAGNOSIS:
Pretibial Myxedema
DISCUSSION:
Localized, or pretibial, myxedema occurs most commonly in females, ages 20-40 years old. It represents one of the signs of Graves’ disease, where the dermopathy will typically present one year after ophthalmopathy. It is characterized by cutaneous induration of the shins, due to mucin deposition, and represents one of the cutaneous findings in patient’s with Graves’ disease. It is a systemic subcutaneous condition that becomes clinically apparent in the lower extremities due to local factors such as dependent position and mechanical stress. Our patient had a known history of Graves’ disease, however, she presented with lower extremity dermopathy several years after successful treatment and normalization of thyroid hormones.
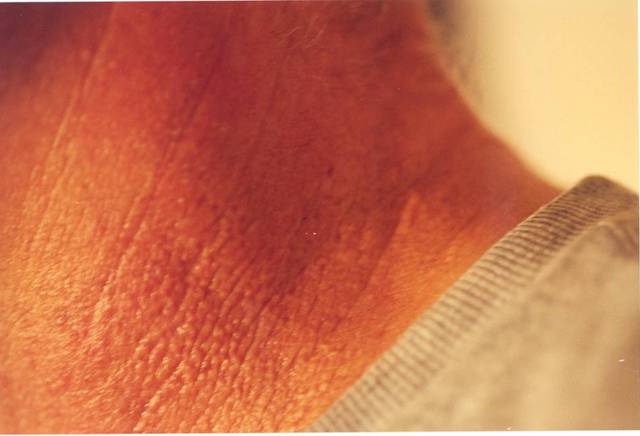
Clinically, it presents as erythematous to flesh-colored, purple-brown or yellowish, waxy indurated nodules or plaques on anterolateral aspect of lower legs or feet, typically symmetric. There is an associated diffuse, non-pitting edema of the shins or feet, due to dermal mucin retaining fluid, which can ultimately evolve into elephantiasis. Often seen is the characteristic peau d’orange or pigskin appearance. The lesions are typically asymptomatic and only of cosmetic concern, however, functional impairment can occur, such as difficulty wearing shoes. The first sign of the disease may be great toe involvement secondary to trauma caused by shoes. Overall, the pathogenesis is due to glycosaminoglycans accumulating in the dermis and subcutaneous tissues. This is thought to be a result of immunologic manifestations of TSH receptor antibodies, sensitized T lymphocytes and cytokine release, as well as mechanical trauma leading to activation of the antigen-specific response.
TREATMENT:
First-line treatment options including topical corticosteroids under occlusion and intralesional kenalog did not improve her symptoms. Off-label treatment with hyaluronidase injections into her enlarged great toes led to significant improvement in signs, symptoms, and overall patient comfort and satisfaction.
For our patient, clobetasol ointment was prescribed twice daily to the affected areas under occlusion, monthly ILTAC 10mg/cc distributed evenly to nodules on R pretibial region and bilateral great toes, and compression stockings 20-30mmHg daily with leg elevation while at rest. Additional treatment included 0.3cc of hyaluronidase diluted with 1% lidocaine in a 1:1 ratio, injected as evenly distributed aliquots into the great toes. Pentoxifylline 400mg PO twice daily was given for two days, however, it was discontinued as the patient could not tolerate the medication.
REFERENCES:
Antonelli, A., et al. (1994). Pretibial myxedema and high-dose intravenous immunoglobulin treatment. Thyroid, 4(4), 400-408. https://doi.org/10.1089/thy.1994.4.400 [PMID: 7847978]
Bolognia, J. L., Jorizzo, J. L., & Rapini, R. P. (2008). Dermatology (2nd ed., pp. 616-618). Elsevier.
Elston, D., & Ferringer, T. (2008). In Requisites in Dermatology: Dermatopathology (pp. 227-228). Elsevier.
Engin, B., et al. (2007). Successful combined pentoxifylline and intralesional triamcinolone acetonide treatment of severe pretibial myxedema. Dermatology Online Journal, 13(6). Retrieved from https://escholarship.org/uc/item/8m78d8qs
Fatourechi, V. (2005). Pretibial myxedema: Pathophysiology and treatment options. American Journal of Clinical Dermatology, 6(5), 295-309. https://doi.org/10.2165/00128071-200506050-00003 [PMID: 16181026]
Gardner, K. (2014). Pretibial myxedema. Retrieved from http://dermnetnz.org/dermal-infiltrative/pretibial-myxoedema.html
Heyes, C., Nolan, R., Leahy, M., & Gebauer, K. (2012). Treatment-resistant elephantiasic thyroid dermopathy responding to rituximab and plasmapheresis. Australasian Journal of Dermatology, 53, e1-4. https://doi.org/10.1111/j.1440-0960.2011.00782.x [PMID: 22107634]
Lebwohl, M., Heymann, W., Berth-Jones, J., & Coulson, I. (2014). Treatment of Skin Disease: Comprehensive Therapeutic Strategies (4th ed., pp. 612-614). Elsevier.
Shinohara, M., Hamasaki, Y., & Katayama, I. (2000). Refractory pretibial myxedema with response to intralesional insulin-like growth factor 1 antagonist (octreotide): Downregulation of hyaluronic acid production by the lesional fibroblasts. British Journal of Dermatology, 143, 1083-1086. https://doi.org/10.1046/j.1365-2133.2000.03794.x [PMID: 11012498]
Von Hilsheimer, G. E. (2014). Pretibial myxedema. Retrieved from http://emedicine.medscape.com/article/1103765-overview