Two Brown Spots on the Left Hand
Presenter: Matthew Muellenhoff , DO, Thi Tran, DO, Frank Armstrong , DO, Kathleen Soe, DO, Greg Houck, DO, Marya Cassandra, DO
Dermatology Program: Sun Coast Hospital, NOVA Southeastern University Dermatology Program
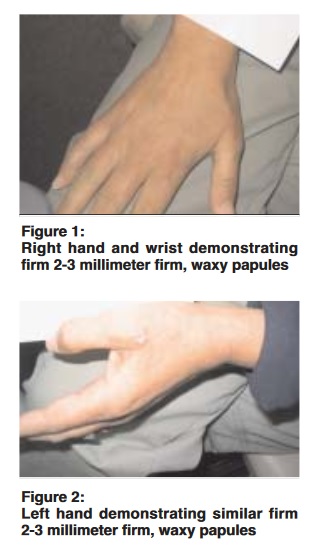
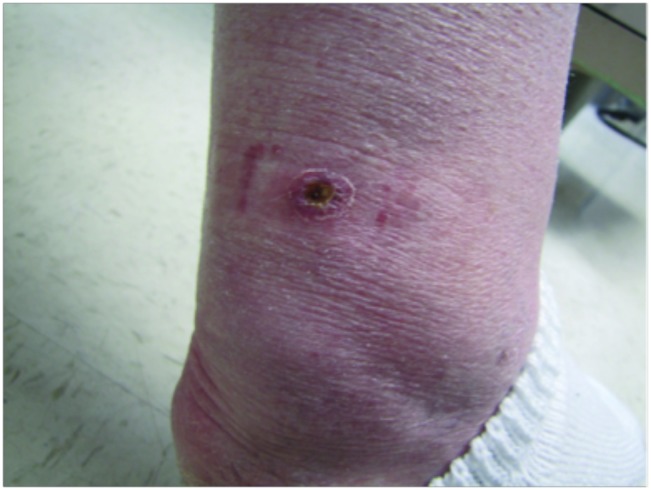
CHIEF COMPLAINT: Two Brown Spots on the Left Hand
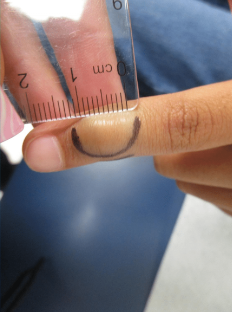
CLINICAL HISTORY: The patient reported a 5-year history of two brown spots on the left hand. Initially, the lesions were blue and attributed to ink stains although the patient denied contact with any staining chemicals or dyes. The “spots” increased in size over a two-year period and changed from blue to brown in color. She denied recent travel and had no history of skin cancer or atypical nevi. Family history revealed a brother with a history of melanoma. Her medications included premarin and glucosamine and she denied any allergies.