CORRECT DIAGNOSIS:
Wegener’s Granulomatosis
DISCUSSION:
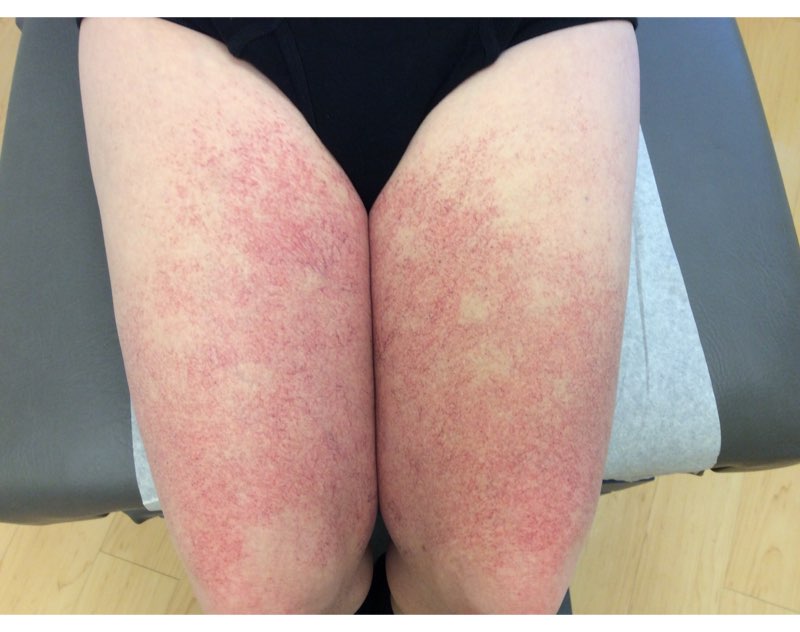
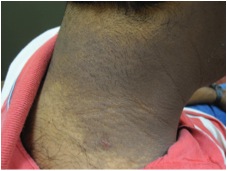
Wegener’s Granulomatosis is an idiopathic systemic vasculitis with classic involvement of the upper and lower respiratory tracts and the kidneys, yet any organ system can be involved. Cutaneous manifestations of Wegener’s Granulomatosis are uncommon as the initial presentation, occurring in only 13 percent, but are present in 30-50 percent of patients throughout the course of the disease. The skin lesions are non-specific and include palpable purpura, necrotizing ulcers, papules, nodules, vesicles, bullae, petechiae, pustules, macules, pyoderma gangrenosum, erythema, and ecchymosis. Unlike our patient, skin disease is usually minor and rarely dominates the clinical picture. Skin involvement indicates active disease, parallels disease activity in other organs, and usually responds well to treatment. No skin biopsy is diagnostic of Wegener’s Granulomatosis. Only 14-28 percent of skin biopsies demonstrate specific histopathology. There is a stronger correlation between active disease and a specific histopathologic finding. Necrotizing vasculitis is the most frequently reported specific biopsy. Biopsies from other organ systems are no better than skin biopsies, which are easier and less invasive to obtain. The clinical presentation of Wegener’s Granulomatosis is very diverse which may delay the diagnosis. The differential diagnosis includes infections, Henoch Schonlein purpura, Behcet’s syndrome, systemic lupus erythematosus, sarcoid, microscopic polyarteritis, and drug reactions. Although no cutaneous lesion or histopathologic finding is specific for Wegener’s Granulomatosis, together with other clinical and radiographic information, the lesions can facilitate early diagnosis.
TREATMENT:
The actual treatment for this patient:
Prednisone 60mg/day and cyclophosphamide 1.5mg/kg/day. There was significant improvement after 2 weeks of treatment with no new lesions developing. The lesions healed with scarring after 6 weeks of treatment.

REFERENCES:
Hoffman, G. S., Kerr, G. S., Leavitt, R. Y., Hallahan, C. W., Lebovics, R. S., Travis, W. D., et al. (1992). Wegener granulomatosis: An analysis of 158 patients. Annals of Internal Medicine, 116(6), 488–498. https://doi.org/10.7326/0003-4819-116-6-488 [PMID: 1541961]
Fauci, A. S., Haynes, B. F., Katz, P., & Wolff, S. M. (1983). Wegener’s granulomatosis: Prospective clinical and therapeutic experience with 85 patients for 21 years. Annals of Internal Medicine, 98(1), 76–85. https://doi.org/10.7326/0003-4819-98-1-76 [PMID: 6603231]
Daoud, M. S., Gibson, L. E., DeRemee, R. A., Specks, U., el-Azhary, R. A., & Su, W. P. (1994). Cutaneous Wegener’s granulomatosis: Clinical, histopathologic, and immunopathologic features of thirty patients. Journal of the American Academy of Dermatology, 31(4), 605–612. https://doi.org/10.1016/S0190-9622(94)70001-8 [PMID: 7945596]
Patten, S. F., & Tomecki, K. J. (1993). Wegener’s granulomatosis: Cutaneous and oral mucosal disease. Journal of the American Academy of Dermatology, 28(5), 710–718. https://doi.org/10.1016/S0190-9622(08)80563-0 [PMID: 8474601]
Frances, C., Huong Du, L. T., Piette, J. C., Saada, V., Boisnic, S., Wechsler, B., et al. (1994). Wegener’s granulomatosis: Dermatological manifestations in 75 cases with clinicopathologic correlation. Archives of Dermatology, 130(7), 861–867. https://doi.org/10.1001/archderm.130.7.861 [PMID: 8012617]
Hu, C. H., O’Loughlin, S., & Winkelmann, R. K. (1977). Cutaneous manifestations of Wegener’s granulomatosis. Archives of Dermatology, 113(2), 175–182. https://doi.org/10.1001/archderm.113.2.175 [PMID: 838673]
Barksdale, S. K., Hallahan, C. W., Kerr, G. S., Fauci, A. S., Stern, J. B., & Travis, W. D. (1995). Cutaneous pathology in Wegener’s granulomatosis: A clinicopathologic study of 75 biopsies in 46 patients. American Journal of Surgical Pathology, 19(2), 161–172. https://doi.org/10.1097/00000478-199502000-00002 [PMID: 7858558]
Stein, S. L., Miller, L. C., & Konnikov, N. (1998). Wegener’s granulomatosis: Case report and literature review. Pediatric Dermatology, 15(5), 352–356. https://doi.org/10.1111/j.1525-1470.1998.tb00326.x [PMID: 9806918]