CORRECT DIAGNOSIS:
Merkel Cell Carcinoma
DISCUSSION:
Merkel cell carcinoma (MCC) is a rare, aggressive, primary skin cancer exhibiting neuroendocrine differentiation. The histogenesis of MCC is unknown.
The 2-year survival is 50-70% and whites have a 20-fold increased relative risk versus blacks. Some studies show that women have a higher incidence of MCC, but survival is greater in women. The mean age at diagnosis is 75 years old.
MCC usually presents as a solitary, dome-shaped nodule or firm plaque, flesh or red in color often with prominent telangiectasias. MCC is usually limited to the skin, but lymphadenopathy, fatigue, weight loss, or hemoptysis should prompt a search for metastasis. Most lesions are found on the head or neck. A chest X-ray or CT scan is helpful in ruling out oat cell carcinoma of the lung with cutaneous metastasis.
Histologic Findings: Tumors cells usually are located intradermally; an intraepidermal component also may be present, and a purely intraepidermal (in situ) MCC rarely may be encountered. Reactive epidermal hyperplasia is frequent. The tumor is composed of round, small, dark cells within conspicuous nucleoli and generally open chromatin with peripheral heterochromatin (“salt and pepper” pattern). Mitotic figures and apoptotic bodies often are numerous.
Several architectural patterns of an intradermal tumor are recognized. The classic trabecular pattern consists of interconnecting strands of tumor cells in the dermis, with the formation of cellular aggregates resembling glands or neural rosettes. The intermediate pattern is the most common and exhibits large, solid nests of neoplastic cells. The least common, diffuse pattern consists of the infiltration of tumor cells among dermal collagen bundles, without the more distinctive organoid appearance of the trabecular pattern. A particular tumor often will contain elements of all architectural patterns, with individual variation in the proportions represented.
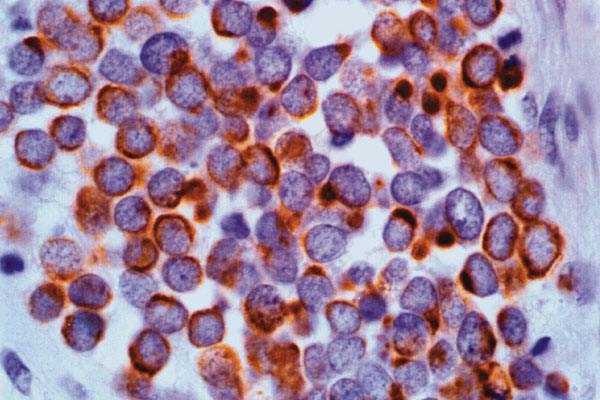
Immunohistochemistry is very helpful. Cytokeratin 20 is expressed in a dot-like para-nuclear or crescentic pattern. The CK20 expression is so sensitive and specific that it has largely replaced traditional markers of neuroendocrine differentiation. Staining with CK20 is considered a finding that rules against the possibility of oat cell carcinoma of the lung. See the digital photomicrograph of positive CK20 staining in the para-nuclear dot or crescentic pattern below.
TREATMENT:
Work-up should include a search for metastasis, regional nodal metastasis being the most common. Wide local excision (3 cm) or Mohs micrographic surgery are both acceptable options for excision, and adjuvant radiation therapy is warranted as well.
Our patient received excision via Mohs surgery with clear margins. However, because the tumor cells of Merkel cell carcinoma may be discontiguous, adjuvant radiation therapy was performed as well.
REFERENCES:
Shea, C. R., et al. (2003). Merkel cell carcinoma. eMedicine. Retrieved from https://emedicine.com
Elder, D. E., et al. (1997). Lever’s histopathology of the skin (8th ed., pp. 719–796). Philadelphia: Lippincott.
Miettinen, M. (1995). Keratin 20: Immunohistochemical marker for gastrointestinal, urothelial, and Merkel cell carcinomas. Modern Pathology, 8(4), 384–388. https://doi.org/10.1038/modpathol.3880146 [PMID: 7738569]
O’Connor, W. J., Roenigk, R. K., & Brodland, D. G. (1997). Merkel cell carcinoma: Comparison of Mohs micrographic surgery and wide excision in eighty-six patients. Dermatologic Surgery, 23(10), 929–933. https://doi.org/10.1111/j.1524-4725.1997.tb00448.x [PMID: 9322148]
Meeuwissen, J. A., Bourne, R. G., & Kearsley, J. H. (1995). The importance of postoperative radiation therapy in the treatment of Merkel cell carcinoma. International Journal of Radiation Oncology Biology Physics, 31(2), 325–331. https://doi.org/10.1016/0360-3016(94)00360-B [PMID: 7818782]
Solares, J., & Salinas, V. (1998). Primary neuroendocrine (Merkel cell) carcinoma of the eyelid. Archivos de la Sociedad Española de Oftalmología, 73(10), 629–631.




