CORRECT DIAGNOSIS:
Contact dermatitis
DISCUSSION:
The goal of this case is to trust the findings of your physical exam. One would certainly not want to miss the diagnosis of orbital cellulitis or herpes zoster ophthalmicus- but there was nothing in the history or physical exam to support these diagnoses.
Orbital cellulitis often results from contiguous spread from the paranasal sinuses. There is often a preceding history of URI or sinusitis. The presentation often includes pain, erythema, proptosis, decreased motility and acuity, afferent pupillary defect, fever, and leukocytosis. Usually, blood cultures are negative. Complications include septic cavernous sinus thrombosis and meningitis. This requires a hospital admission with STAT Ophthalmology consult, IV antibiotics, orbital imaging, and appropriate lab work.
Preorbital cellulitis presents with pain and erythema around the orbit without the ophthalmologic symptoms. As above, an Ophthalmology consult is needed with appropriate antibiotics, imaging, and careful monitoring for the progression to orbital cellulitis.
Blepharitis is inflammation of the eyelids, usually in association with rosacea or seborrheic dermatitis. The eyelid margins are greasy, ulcerated, and crusty. These ulcers are usually colonized with staphylococcus. Treatment involves addressing the underlying condition, warm compresses, and topical antibiotics.
Herpes Zoster Ophthalmicus represents V1 nasocilliary branch involvement of varicella zoster virus reactivation. Multiple lesions in various stages of development (vesicles, pustules, erosions, crusts) grouped in a herpetic distribution along one dermatome are characteristic. Often, the classic vesicle on erythematous base can involve the tip of the nose (Hutchinson’s sign). An ophthalmologic evaluation is needed to evaluate corneal involvement. The diagnosis is clinical, although a Tzanck smear or PCR can be utilized to confirm. Therapy is antivirals, cycloplegics, and possibly corticosteroids.
TREATMENT:
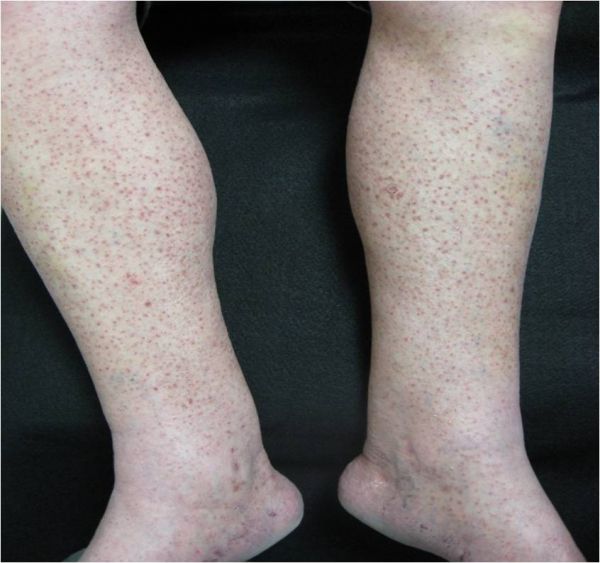
The diagnosis of allergic contact (eyelid) dermatitis was made in this case based on the history and physical exam. Allergic contact dermatitis is the result of type IV delayed hypersensitivity reaction to a previously sensitized allergen. Histopathologic features of acute allergic contact dermatitis include spongiosis, intraepidermal vesicles, bullae, and exocytosis of lymphocytes. There is a mixed dermal infiltrate including a variable amount of eosinophils. (fig. 3A). Chronically these features are replaced by psoriasiform hyperplasia (fig. 3B).
Eyelid dermatitis may be caused by atopic dermatitis, substances transferred to the eyelid from the hands (nail polish), cosmetics, or hair products. The patient was instructed to discontinue all topical therapy, apply pimecrolimus cream BID, and to follow up the following day to check progress and to bring in the topical medicines she had been using. The patient was instructed to notify the office immediately if she experienced any fever or ophthalmologic symptoms. The following day, the patient reported she had been using Neosporin:
Active Ingredients: Each gram contains: Polymyxin B Sulfate (5,000 units), Bacitracin Zinc (400 units), Neomycin (3.5 mg)
Inactive Ingredients: Cocoa Butter, Cottonseed Oil, Olive Oil, Sodium Pyruvate, Tocopheryl Acetate, White Petrolatum
The patient was informed she likely had an allergic response to neomycin, as it is the most common sensitizer among topical antibiotics. Co-reactivity is commonly seen between neomycin and bacitracin; this is due to co-sensitization from their frequent use in combination rather than cross-reactivity. Neomycin and bacitracin were added to her allergy list and at six weeks her eczematous patch had evolved into post-inflammatory hyperpigmentation.

REFERENCES:
Odom, R. B., et al. (2000). Andrew’s diseases of the skin: Clinical dermatology (9th ed.). Philadelphia: W. B. Saunders Co.
Bolognia, J. L., et al. (2003). Dermatology (1st ed.). Philadelphia: Mosby.
Braunwald, E., et al. (2001). Harrison’s principles of internal medicine (15th ed.). New York: McGraw Hill.
Albert, M. R., Gonzalez, S., & Gonzalez, E. (1998). Patch testing reactions to a standard series in 608 patients tested from 1990 to 1997 at Massachusetts General Hospital. American Journal of Contact Dermatology, 9(4), 207-211.