CORRECT DIAGNOSIS:
Urticaria Pigmentosa
DISCUSSION:
Mastocytosis (MC) is a heterogeneous group of disorders characterized by abnormal proliferation and accumulation of mast cells in the skin, bone marrow, gastrointestinal tract, liver, spleen, and lymph nodes. The spectrum of mast cell disease has been classified based on the type and extent of involvement as well as the age of onset.
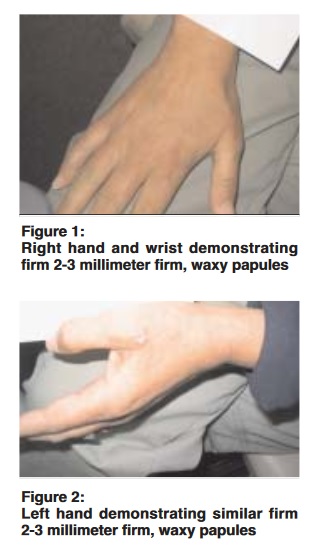
Cutaneous forms include solitary mastocytoma, urticaria pigmentosa, diffuse cutaneous mastocytosis, and telangiectasia macularis eruptiva perstans. Urticaria pigmentosa is the most common form of cutaneous MC. Urticaria pigmentosa (UP) usually presents in childhood and can persist into adulthood, however, most spontaneously improve. Patients with UP may also experience various systemic symptoms such as pruritus, flushing, dizziness, palpitations, syncope, nausea, diarrhea, abdominal pain, headache, musculoskeletal pain, and neuropsychiatric disturbances.
Serum tryptase levels and 24-hour urine histamine metabolites are the most useful lab test for MC. High levels of soluble CD117 and CD25 receptors are strongly associated with the severity of bone marrow involvement. MC can be associated with mutations in codon 816 c-kit, a proto-oncogene that encodes for KIT, the receptor for stem cell factor. This mutation may contribute to an increased rate of mast cell proliferation.
TREATMENT:
Therapy is aimed at minimizing signs and symptoms related to histamine release. This includes avoiding triggers, H1/H2 antagonists, oral cromolyn sodium, PUVA, and topical/intralesional steroids.
REFERENCES:
1. Bolognia JL, Jorizzo JL, Rapini RP, et. al. (2003) Dermatology. Spain: Mosby
2. Schwartz LB – Immunol Allergy Clin North Am – 01-AUG-2006; 26(3): 451-63
3. Shaffer HC – J Am Acad Dermatol – 01-MAY-2006; 54(5 Suppl): S210-3
4. Valent P – Immunol Allergy Clin North Am – 01-AUG-2006; 26(3): 515-34
5. Bishop AB – J Am Acad Dermatol – September 2006; 55(3); 553-556
Additional Comment:
As noted in our patient, extensive workup has not revealed any evidence of systemic disease. Despite her relatively low mast cell burden, normal tryptase level, and negative bone marrow biopsy, she continues to have symptoms even with aggressive medical therapy. Our case supports the literature in that there is little correlation between clinical extent of disease and severity of symptoms. This patient will be closely monitored in conjunction with an allergist, as there is a risk of progression into more aggressive disease. Repeat bone marrow biopsy should be considered if tryptase level trends upward.