Presenter: Wade Keller, DO
Dermatology Program: Kingman Regional Medical Center/Midwestern University
Program Director: Don Anderson, DO
Submitted on: March 31, 2008
CHIEF COMPLAINT: Pruritic rash to both arms and upper back
CLINICAL HISTORY: A 79-year-old female presented with a 2 weeks history of a progressively worsening pruritic rash that began on her right upper arm then the left arm and upper back. She is not sure if light makes the rash worse. She denies any changes in her medications with the exception of the addition of lisinopril three months ago. No previous treatmetns. Current medications include Lisinopril, Lipitor, Pacerone, Timolol, Aspirin, Xalantin, and Timoptic.
PHYSICAL EXAM:
An elderly appearing female with multiple annular and arciform nonindurated plaques with trailing scale and lacking follicular plugging affecting the lateral aspects of the arms bilaterally and the upper back. She is afebrile and without lymphadenopathy.



LABORATORY TESTS:
ANA + (1:320, Nucleolar pattern), SS-A antibody > 8.0 positive, SS-B antibody 1.0 positive, ds-DNA antibody negative, SCL-70 negative, Anti-Histone negative. CBC, Liver, and Renal functions all within normal limits.
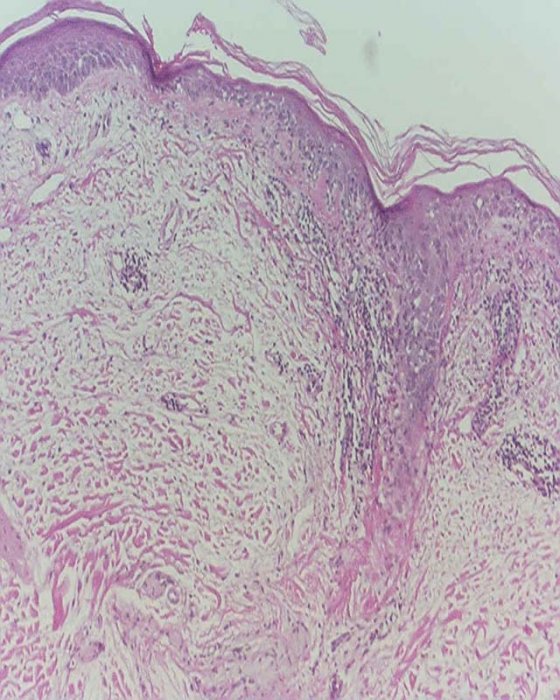
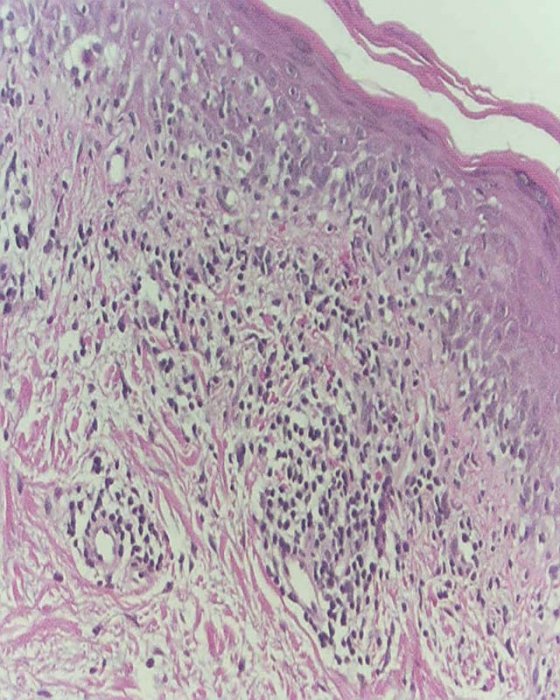
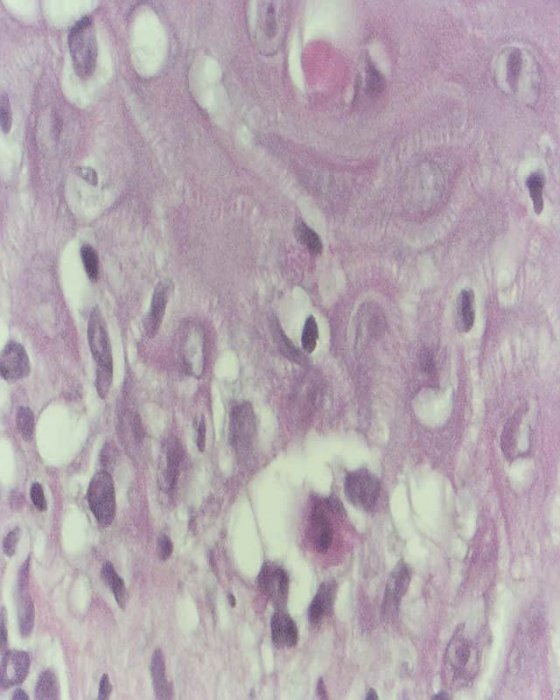
DERMATOHISTOPATHOLOGY:
Two 5 mm punch biopsies were performed. The first punch biopsy was on the outer border of an annular plaque of the right arm for H&E. The second was a perilesional biopsy of normal-appearing skin from the left arm for Direct Immunofluorescence (DIF).
A DIF image was not available, but it demonstrated linear and granular deposits of IgG, IgA, and IgM, along with C3, at the dermal-epidermal junction and extending into the superficial dermis.
The H&E reveals slight hyperkeratosis overlying a focally acanthotic but focally flattened epidermis. A superficial perivascular and somewhat lichenoid lymphocytic inflammatory infiltrate with exocytosis of lymphocytes into the epidermis. Scattered necrotic keratinocytes are seen. A PAS stain does not reveal significant thickening of the dermal-epidermal junction basement membrane, and fungal organisms are absent. A colloidal iron stain demonstrates mildly increased reticular dermal mucin.
DIFFERENTIAL DIAGNOSIS:
1. Erythema Annulare Centrifugum
2. Tinea Corporis
3. Psoriasis
4. Subacute Cutaneous Lupus Erythematosus
5. Granuloma Annulare




