CORRECT DIAGNOSIS:
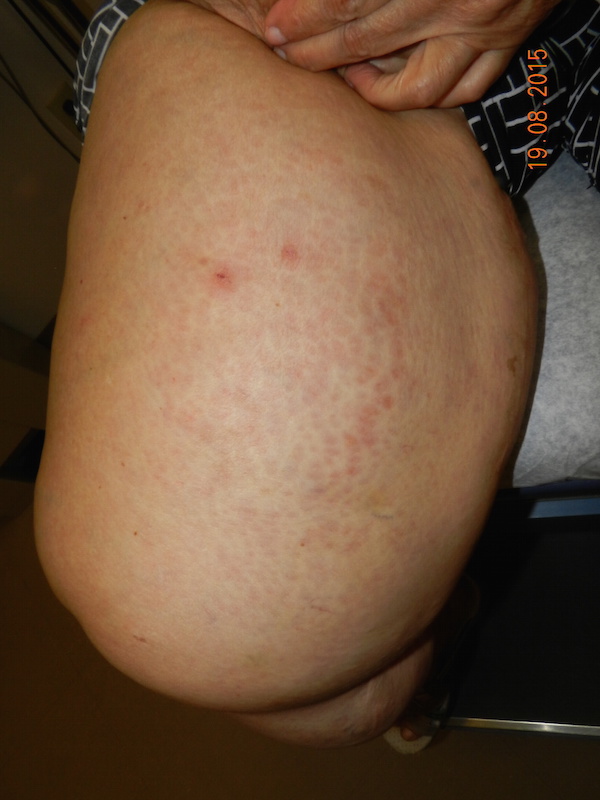
Subacute Cutaneous Lupus Erythematosus
DISCUSSION:
Subacute Cutaneous Lupus Erythematosus (SCLE) is a recurring, photosensitive, nonscarring, nonindurated, and superficial lesion with two primary forms, annular and/or papulosquamous. It may be seen in patients ranging from 1 � years of age to the elderly, but it primarily affects Caucasian females in the 4th decade. It is uncommonly seen in African-American, Chinese, and Korean populations. SCLE affects the extensor arms & shoulders, upper trunk and “V” of the neck as well as forearms and dorsal hands usually sparing the knuckles and rarely involving the face. On photochallenge testing, 100% of SCLE patients had abnormal reactions to ultraviolet light. SCLE is associated with HLA-A1, B8, and DR3 as well as deficiency or lack of C2 or C4. Also, a new genetic association exists in a single nucleotide polymorphism in a gene promoter region for TNF-α.
The proposed pathogenesis progresses through four sequential stages. A genetically susceptible individual experiences a loss of self-tolerance/autoimmunity induction. The autoimmune process expands, culminating in tissue injury, and the manifestation of the disease. Histologically, it is common to see epidermal atrophy. The basal layer keratinocytes appear hydropic or have eosinophilic degeneration. The upper dermis demonstrates a sparse interface and perivascular lymphohistiocytic infiltrate. On direct immunofluorescence of 60% of SCLE cases, a granular band of immunoglobulin and complement is seen at the dermo-epidermal junction (DEJ). Alternatively, a dust-like deposition of IgG can be seen over epidermal basal cells and below the DEJ.
Drug-induced autoantibody production was appreciated in 1985, and these autoantibodies were of the Ro/SS-A type. Seventy percent of patients with SCLE have antinuclear antibody and Ro/SS-A positivity. Autoantibodies to La/SS-B are also common. Less commonly seen are autoantibodies to double-stranded DNA and Smith. Today, many common medications have been associated with the development of SCLE lesions, including calcium channel blockers, diuretics, angiotensin-converting enzyme inhibitors, antihistamines, seizure medications, antimalarials, sulfonylureas, chemotherapeutics, and others to include etanercept and infliximab.
Of the patients with SCLE lesions, 20% will develop either discoid or acute cutaneous LE lesions. Leukocytoclastic vasculitis, Raynaud’s phenomenon, and Livedo reticularis are also seen. Almost half will have 4 or more criteria for systemic lupus erythematosus (SLE), but they usually lack renal and CNS disease. Ten to fifteen percent will develop SLE. Forty-three percent of patients develop Sj�gren�s syndrome, which also has Ro/SS-A autoantibodies. Other disease associations with SCLE include autoimmune thyroiditis, hereditary angioedema, and autoimmune polyglandular syndrome type II.
TREATMENT:
Treatment of SCLE emphasizes photoprotection by way of avoidance and broad-spectrum sunscreens. Topical corticosteroids, tacrolimus, and pimecrolimus are also effective for improving the SCLE lesions. Systemic therapy with hydroxychloroquine, chloroquine, or quinacrine is effective in 75% of patients. Interestingly, these medications are ineffective in cigarette smoking patients. Thalidomide is also effective, but its use is limited due to toxicity. Dapsone, clofazimine, and gold formulations have been used also. Methotrexate, Azathioprine, and mycophenolate mofetil can be considered in recalcitrant cases.
REFERENCES:
Sontheimer, R. D. (2005). Subacute cutaneous lupus erythematosus: 25-year evolution of a prototypic subset (subphenotype) of lupus erythematosus defined by characteristic cutaneous, pathological, immunological, and genetic findings. Autoimmunity Reviews, 4, 253-263. PMID: 15863132
Werth, V. P. (2005). Clinical manifestations of cutaneous lupus. Autoimmunity Reviews, 4, 296-302. PMID: 15882996
Franceschini, F., & Cavazzana, I. (2005). Anti-Ro/SSA and La/SSB antibodies. Autoimmunity, 38(1), 55-63. PMID: 15704526
Tebbe, B. (2004). Clinical course and prognosis of cutaneous lupus erythematosus. Clinics in Dermatology, 22, 121-124. PMID: 14751305
Albrecht, J., Berlin, J. A., Braverman, I. M., et al. (2004). Dermatology position paper on the revision of the 1982 ACR criteria for systemic lupus erythematosus. Lupus, 13, 839-849. PMID: 15520037
Chlebus, E., Wolska, H., Blaszczyk, M., & Jablonska, S. (1998). Subacute cutaneous lupus erythematosus versus systemic lupus erythematosus: Diagnostic criteria and therapeutic implications. Journal of the American Academy of Dermatology, 38, 405-412. PMID: 9488617
Sontheimer, R. D., Thomas, J. R., & Gilliam, J. N. (1979). Subacute cutaneous lupus erythematosus: A cutaneous marker for a distinct lupus erythematosus subset. Archives of Dermatology, 115, 1409-1415. PMID: 489315
Additional Comment: The author would like to thank Steven Ruhoy, MD for providing the histology images.