CORRECT DIAGNOSIS:
Radiation Dermatitis
DISCUSSION:
Radiographic procedures performed worldwide has increased practically every year. In the United States alone, there were over 4.21 million interventional fluoroscopic procedures in 2006 versus 700,000 in 1996. The incidence of radiation dermatitis has increased, however, the number of reported cases appears much smaller than might be expected. There have been fewer than 100 fluoroscopically-induced cases reported in the literature to date. This is most likely due to the difficulty in diagnosing this condition. Lesions ranging from simple erythema to transient alopecia, telangiectasia, atrophy, hyperpigmentation, hypopigmentation, necrosis, chronic ulceration, and squamous cell carcinoma have all been described.
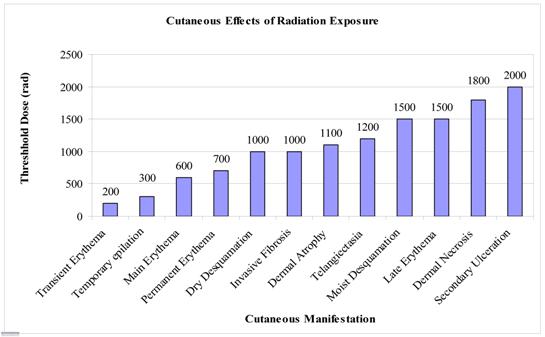
In a recent review of 73 patients, initial diagnoses as disparate as fixed-drug eruption, morphea, contact dermatitis, infection, and spider-bite were made. Lesions have appeared anywhere from less than 1 day to 10 years after the causative procedure. Improved physician education and awareness have led to both higher rates of diagnoses as well as better prevention. Frazier et al in 2007 most recently summarized the known changes to skin observed with increasing dosages of radiation.
To prevent radiation-induced injury, the radiation dose to affected areas of skin should be monitored in real-time and kept below these levels. Emphasis must be placed on detection. Taking a detailed history is absolutely essential. Most patients do not offer a prior history of fluoroscopy, either because they assume it irrelevant or have forgotten it completely (2,3,4). Histopathology is of limited utility as specimens are often non-diagnostic without proper clinical correlation. Due to poor wound healing, biopsies are discouraged biopsies in these cases4.
TREATMENT:
Biafine topical emulsion allowed the biopsied area to heal well. It is only with a high index of suspicion and specific questioning that many of these mysterious cases with a long latent period can be solved. With improved physician awareness, it will hopefully be solved more frequently.
REFERENCES:
Barnea, Y., Amir, A., Shafir, R., Weiss, J., & Gur, E. (2002). Chronic radiodermatitis injury after cardiac catheterization. Annals of Plastic Surgery, 49(6), 668-672. PMID: 12439632
Sajben, F., Schoelch, S., & Barnette, D. (1999). Fluoroscopic-induced radiation dermatitis. Cutis, 64, 57-59. PMID: 10429383
Frazier, T., Richardson, J., Fabre, V., & Callen, J. (2007). Fluoroscopy-induced chronic radiation skin injury. Archives of Dermatology, 143, 637-640. PMID: 17563007
Koenig, T., Wolff, D., Mettler, F., & Wagner, L. (2001). Skin injuries from fluoroscopically guided procedures: Part 1, characteristics of radiation injury. American Journal of Radiology, 177, 3-11. PMID: 11448759
Market Research Cardiac Catheterization Products Overview. (2007). Retrieved October 30, 2007, from http://www.imvinfo.com/index.aspx?sec=ccath&sub=def
Dehen, L., Vilmer, C., Humiliere, C., Corcos, T., Pentousis, D., Ollivaud, L., Chatelain, D., & Dubertret, L. (1999). Chronic radiodermatitis following cardiac catheterization: A report of two cases and a brief review of the literature. Heart, 81, 308-312. PMID: 10377300
Schecter, A., Lewis, M., Robinson-Boston, L., & Pan, T. (2003). Cardiac catheterization-induced acute radiation dermatitis presenting as a fixed drug eruption – Case reports. Journal of Drugs in Dermatology, 2(4), 425-427. PMID: 15227475
Wagner, L., McNeese, M., Marx, M., & Siegel, E. (1999). Severe skin reactions from fluoroscopy: Case report and review of the literature. Radiology, 213, 773-776. PMID: 10587839
Aerts, A., Decraene, T., Van Den Oord, J., Dens, J., Janssens, S., Guelinckx, P., Flour, M., Degreef, H., & Garmyn, M. (2003). Chronic radiodermatitis following percutaneous coronary interventions: A report of two cases. Journal of the European Academy of Dermatology and Venereology, 17, 340-343. PMID: 12755956




