CORRECT DIAGNOSIS:
Acquired perforating dermatosis secondary to renal failure
DISCUSSION:
The perforating dermatoses have classically been divided into four main entities: Kyrle’s disease, perforating folliculitis, reactive perforating collagenosis, and elastosis perforans serpiginosa. Acquired perforating dermatosis (APD), as described by Rapini et al., has recently become recognized as a separate disease entity within the category of perforating dermatoses. APD is seen almost exclusively in patients who have chronic renal failure, diabetes mellitus, or both, but has been reported in patients with neither disease. APD has been reported to occur in approximately 10% of hemodialysis patients, with the onset of lesions anywhere from 1 to 5 years after the start of dialysis.
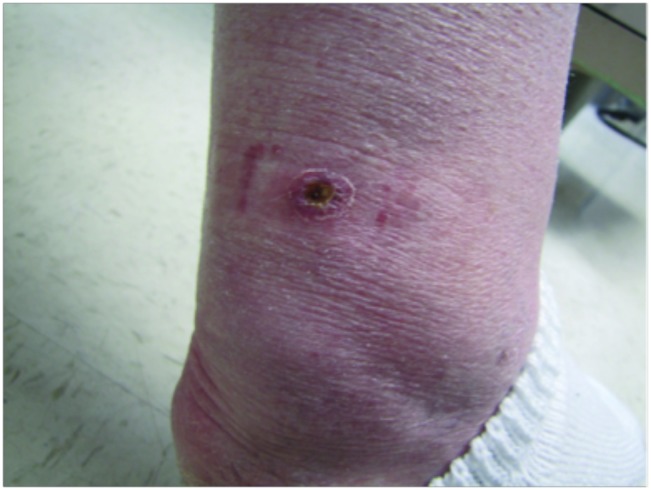
Clinically, APD presents as pruritic papules often with a central keratotic plug, commonly appearing on the extensor extremities and trunk. The lesions may progress to nodules or plaques that may resemble prurigo nodularis, and Koebnerization may be seen. The exact mechanism behind APD in renal failure and diabetic patients is not known. Some authors have described APD as a reaction to trauma and scratching related to the associated pruritus, while others have theorized that it may be a result of microangiopathy caused by the associated renal failure or diabetes. Diagnosis is made based on clinical and histopathological examination.
Histologic examination lies somewhere along a spectrum of patterns that may be found in any of the other major perforating disorders including Kyrle’s disease, perforating folliculitis, elastosis perforans serpiginosa, and reactive perforating collagenosis. The most common pattern is one similar to that of perforating folliculitis showing a disruption in the follicular epithelium often filled with a plug of compact orthokeratosis and parakeratosis. Altered collagen and elastic fibers are commonly seen adjacent to the perforation and can be seen extruding through the perforation. A mixed inflammatory infiltrate of neutrophils, histiocytes, and lymphocytes is often seen in a perifollicular distribution. There may be some histologic overlap with the features of prurigo nodularis.
TREATMENT:
Treatment of APD is often difficult and inadequate. To date, few controlled studies have been done on the various methods used to treat APD. Antihistamines provide little to no relief of the often associated severe pruritus. Some studies and case reports have shown that UVB may provide significant improvement in the pruritus and skin lesions of APD. Other studies have shown response to topical steroids, topical retinoic acid, as well as systemic allopurinol, etretinate, isotretinoin, and the tetracycline family of antibiotics. Complete resolution of lesions and symptoms has been reported after renal transplantation in some patients.
The patient was initially treated with a high potency steroid and oral antihistamines to control itching. We discussed using narrow-band UVB, however, the patient died one month later.
REFERENCES:
Elder, D., Elenitsas, R., Jaworsky, C., & Johnson, B. (2005). Lever’s Histopathology of the Skin (9th ed., pp. 404-408). Lippincott Williams & Wilkins.
Hong, S. B., Park, J. H., Ihm, C. G., & Kim, N. I. (2004). Acquired perforating dermatosis in patients with chronic renal failure and diabetes mellitus. Journal of Korean Medical Science, 19, 283-288. PMID: 15112869
James, W. D., Elston, D. M., Treat, J. R., & Rosenbach, M. A. (2011). Andrews’ Diseases of the Skin (10th ed., pp. 774-775). Elsevier.
Rapini, R. P., Herbert, A. A., & Drucker, C. R. (1989). Acquired perforating dermatosis: Evidence for combined transepidermal elimination of both collagen and elastic fibers. Archives of Dermatology, 125, 1074-1078. PMID: 2768117
Saray, Y., Seckin, D., & Bilezikci, B. (2006). Acquired perforating dermatosis: Clinicopathological features in twenty-two cases. Journal of the European Academy of Dermatology and Venereology, 20(6), 679-688. PMID: 16941645
Ohe, S., Yamamoto, T., & Nakajima, H. (2004). Treatment of acquired perforating dermatosis with narrowband ultraviolet B. Journal of the American Academy of Dermatology, 50(6), 892-894. PMID: 15153046