CORRECT DIAGNOSIS:
Hyperkeratosis lenticularis perstans (Flegel’s Disease)
DISCUSSION:
In 1958, Flegel first described a rare keratinization disorder with a predilection for the distal extremities of adults named hyperkeratosis lenticularis perstans or Flegel’s disease.1 The name hyperkeratosis lenticularis perstans (HLP) refers to the disc or lens shape (lenticularis) of the papules and their persistent nature (perstans). To date, all reports of HLP have been in Caucasian patients with no apparent gender predilection. Most cases have been reported in Europe, with the international incidence similar to that seen in the United States. Onset is during adulthood with red-brown keratotic lesions that are symmetrically distributed, and usually symptomatic and chronic. HLP is occasionally associated with endocrine diseases and neoplasias. Some authors have implicated exposure to ultraviolet (UV) light as a precipitating factor. Others have suggested that cell-mediated cytotoxicity against epithelial cells may be involved. Lesions are not evident until mid-to-late adulthood but have been described in individuals as young as 13 years of age. Thus far, there is no clear understanding of the pathogenesis of HLP.
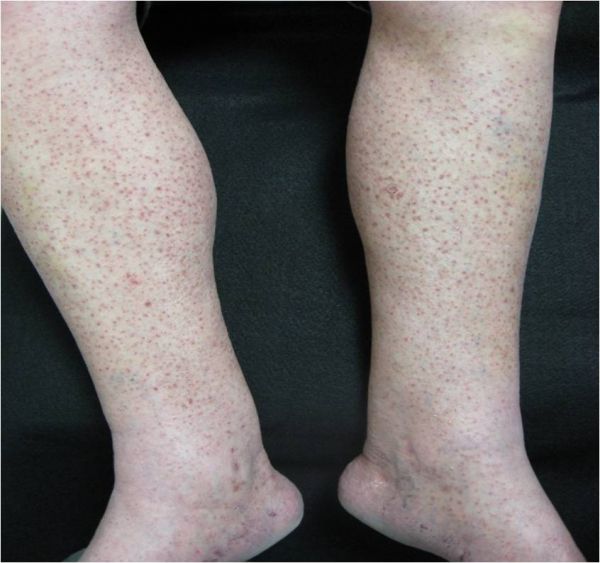
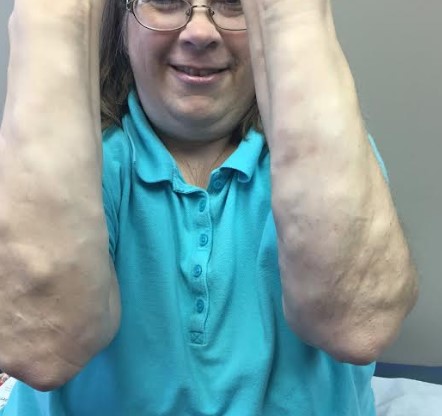
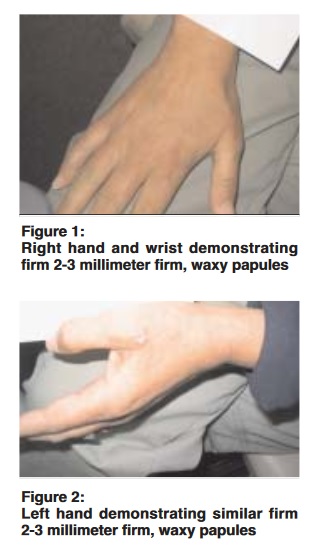
HLP presents clinically with red-brown papules, most often covered by the focal horny scale. Individual papules of HLP measure between 1-5 mm in diameter and generally are up to 1 mm in depth (height). Papules of HLP are primarily located on the dorsal feet and lower legs and are less likely to manifest proximally. This disorder has also been known to involve the thighs, hands, forearms, trunk, ears, and oral mucosa. Lesions of HLP are typically distributed symmetrically, however, unilateral cases have been reported. Involvement of the trunk has been reported as an unusual variant. The ear pinna, arms, palms, plantar surfaces, and oral mucosa have also been reported, with such areas of involvement considered to be rare. Removal of the scales commonly reveals a bright red base with pinpoint bleeding.
Ultrastructurally, a decrease, malformation, or absence of membrane-coating granules (Odland bodies) can be observed. Structurally altered Odland bodies, which contain hydrolytic enzymes results in decreased desquamation of the stratum corneum and retention hyperkeratosis. A lymphoid infiltrate with occasional histiocytes in a band-like pattern in the papillary dermis is typically seen. Although the most characteristic feature is an absence or reduction in Odland bodies, this is not always the case. Depending on the stage of the disease, the histopathologic findings can be quite non-specific with older lesions displaying mild hyperkeratosis with little or no inflammatory infiltrate. Studies reveal the presence of many normal-appearing, Odland bodies in the keratinocytes of older HLP lesions, which is not observed in earlier hyperkeratotic lesions.
Clinically, the differential diagnosis may also include disseminated superficial actinic porokeratosis (DSAP). However, this possibility can be ruled out by histopathological examination of the lesion revealed a coronoid lamella at the hyperkeratotic edge of a DSAP lesion. HLP is a diagnosis that requires a high index of clinical suspicion and appropriate histopathologic correlation. Skin biopsy is helpful in excluding other disorders considered in the differential diagnosis.
TREATMENT:
HLP can be problematic to treat due to its persistent nature. It is characteristically resistant to topical corticosteroids and keratolytic agents. Destructive therapies, such as dermal abrasion and shave-excision, have been noted to be more effective. Topical 5-fluorouracil has been shown to be moderately effective in some cases. However, some patients may not tolerate this treatment due to its irritant side effects. Oral retinoids, (etretinate, isotretinoin) have also been shown to be effective, but relapse occurs after treatment is discontinued. Topical retinoids are not as effective. However, isotretinoin 0.05% gel has been reported to produce good results. Other options include psoralen ultraviolet A (PUVA) and topical calcipotriol. Currently, no standard therapy exists and many cases of HLP are refractory to therapy.
In our case of HLP described above, the patient was refractory to multiple treatment regimens including topical corticosteroids and topical 5-fluorouracil. He was subsequently lost to follow up.
REFERENCES:
Bolognia, J. L., Jorizzo, J. L., Rapini, R. P., et al. (2003). Dermatology. Mosby.
Roling, H., & Junkins-Hopkins, J. M. (n.d.). Hyperkeratosis lenticularis perstans (Flegel disease). Medscape. Retrieved from https://www.emedicine.medscape.com
Miranda-Romero, A., Sambucety, P. S., Bajo del Pozo, C., et al. (1998). Unilateral hyperkeratosis lenticularis perstans (Flegel’s disease). Journal of the American Academy of Dermatology, 39(4), 655-657. https://doi.org/10.1016/S0190-9622(98)70251-0 [PMID: 9778919]
Knipper, J. E., Hud, J. A., & Cockerell, C. J. (1993). Disseminated epidermolytic acanthoma. American Journal of Dermatopathology, 15(1), 70-72. https://doi.org/10.1097/00000372-199302000-00012 [PMID: 8431997]
Bean, S. (1969). Hyperkeratosis lenticularis perstans: A clinical, histopathologic, and genetic study. Archives of Dermatology, 99(6), 705-709. https://doi.org/10.1001/archderm.1969.01610120043007
Flegel, H. (1958). Hyperkeratosis lenticularis perstans. Hautarzt, 9(8), 363-364. [PMID: 13534414]
Ando, K., Hattori, H., & Yamauchi, Y. (2006). Histopathological differences between early and old lesions of hyperkeratosis lenticularis perstans (Flegel’s disease). American Journal of Dermatopathology, 28(2), 122-126. https://doi.org/10.1097/01.dad.0000197991.77959.79 [PMID: 16531923]
Miljkovic, J. (2004). An unusual generalized form of hyperkeratosis lenticularis perstans (Flegel’s disease). Wiener Klinische Wochenschrift, 116(Suppl 2), 78-80. https://doi.org/10.1007/s00508-004-0364-3 [PMID: 15239053]
Jang, K., Choi, J., Sung, K., et al. (1999). Hyperkeratosis lenticularis perstans (Flegel’s disease): Histologic, immunohistochemical, and ultrastructural features in a case. American Journal of Dermatopathology, 21(5), 395-398. https://doi.org/10.1097/00000372-199910000-00011 [PMID: 10542569]
Pearson, L. H., Smith, J. G., & Chalker, D. K. (1987). Hyperkeratosis lenticularis perstans (Flegel’s disease): Case report and literature review. Journal of the American Academy of Dermatology, 16(2), 190-195. https://doi.org/10.1016/S0190-9622(87)70088-1 [PMID: 3541526]
De Argila, D., Revenga, F., Rodriguez, J. L., et al. (1994). Hiperqueratosis lenticularis perstans (enfermedad de Flegel): Estudio clínico-patológico de 10 casos. Actas Dermo-Sifiliográficas, 85, 309-315. [PMID: 7857246]
Langer, K., Zonzits, E., & Konrad, K. (1992). Hyperkeratosis lenticularis perstans (Flegel’s disease): Ultrastructural study of lesional and perilesional skin and therapeutic trial of topical tretinoin versus 5-fluorouracil. Journal of the American Academy of Dermatology, 27(5), 812-816. https://doi.org/10.1016/0190-9622(92)70001-V [PMID: 1466332]
Crespo, A., Crespo, V., Sanz, A., et al. (1990). Hiperqueratosis lenticularis perstans. Actas Dermo-Sifiliográficas, 81, 153-155. [PMID: 2301541]
Cooper, S. M., & George, S. (2000). Flegel’s disease treated with psoralen ultraviolet A. British Journal of Dermatology, 142(2), 340-342. https://doi.org/10.1046/j.1365-2133.2000.03471.x [PMID: 10652036]
Bayramgurler, D., Apaydin, R., Dokmeci, S., et al. (2002). Flegel’s disease: Treatment with topical calcipotriol. Clinical and Experimental Dermatology, 27(2), 161-162. https://doi.org/10.1046/j.1365-2230.2002.01183.x [PMID: 11876073]
Additional Comment: Thank you to Narciss Mobini MD who provided dermatopathology services in this case and assistance with obtaining photomicrographs of histologic findings.