CORRECT DIAGNOSIS:
Eumycotic mycetoma
DISCUSSION:
Mycetoma is a chronic, subcutaneous, granulomatous inflammatory disease caused by either a filamentous bacteria (actinomycotic mycetoma) or true fungi (eumycotic mycetoma). It is characterized by the triad of tumefaction, granules, and draining sinus tracks which can ultimately lead to bony deformity (1). Causative organisms are usually acquired from the soil through a direct penetrating injury, often by a splinter or thorn prick (2). Our patient recalled a thorn prick while gardening two months earlier; however many patients do not recall any such trauma to the infection site (3).
Mycetoma can be found worldwide with the highest incidence occurring in tropical and subtropical countries. The incidence is highest in India and Sudan, and large numbers of cases have been reported in Latin America, Mexico, Venezuela, and Brazil (4). Worldwide the most common cause of eumycetoma is Madurella mycetomatis. Our patient grew Pseudoallescheria boydii from his culture, which is the most common causative organism of eumycetoma in the United States (2).
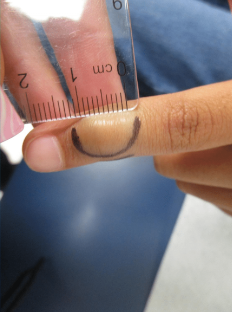
Clinically the infection usually presents on the foot (70-80%) or hand (12%) as a unilateral painless papule or subcutaneous nodule (3,2). As the infection progresses the surrounding tissue becomes swollen, forming multiple draining sinus tracks that express a purulent discharge. Within the purulent discharge are the characteristic grains, also called sclerota, which represent small fungal colonies. Deep subcutaneous abscesses eventually form which extends into the fascia, muscle, and bone, leading to deformity and disability if untreated (2). Histologically, three different types of tissue reactions have been described (3). The organisms can be highlighted with a PAS or methenamine silver stain (GMS).
Correct species identification is important to determine the correct treatment. Tissue culture is the primary method of identification. PCR is an alternate method when tissue cultures are negative (5).
TREATMENT:
The treatment of eumycetoma typically consists of antifungal treatment with either itraconazole or ketoconazole for 18-24 months or longer, combined with surgical excision and debulking (6).
REFERENCES:
McGinnis, M. R. (1996). Mycetoma. Dermatologic Clinics, 14(1), 97-104. https://doi.org/10.1016/S0733-8635(05)70091-3
Lichon, V., & Khachemoune, A. (2006). Mycetoma: A review. American Journal of Clinical Dermatology, 7(5), 315-321. https://doi.org/10.2165/00128071-200607050-00005
Fahal, A. H. (2004). Mycetoma: A thorn in the flesh. Transactions of the Royal Society of Tropical Medicine and Hygiene, 98(1), 3-11. https://doi.org/10.1016/S0035-9203(03)00023-6
Castro, L. G., & Piquero-Casals, J. (2008). Clinical and mycologic findings and therapeutic outcome of 27 mycetoma patients from São Paulo, Brazil. International Journal of Dermatology, 47(2), 160-163. https://doi.org/10.1111/j.1365-4632.2007.03309.x
Borman, A. M., Linton, C. J., Miles, S. J., et al. (2008). Molecular identification of pathogenic fungi. Journal of Antimicrobial Chemotherapy, 61(Suppl. 1), 7-12. https://doi.org/10.1093/jac/dkm433
Ameen, M., & Arenas, R. (2009). Developments in the management of mycetomas. Clinical and Experimental Dermatology, 34(1), 1-7. https://doi.org/10.1111/j.1365-2230.2008.02931.x