CORRECT DIAGNOSIS:
Pilomatricoma
DISCUSSION:
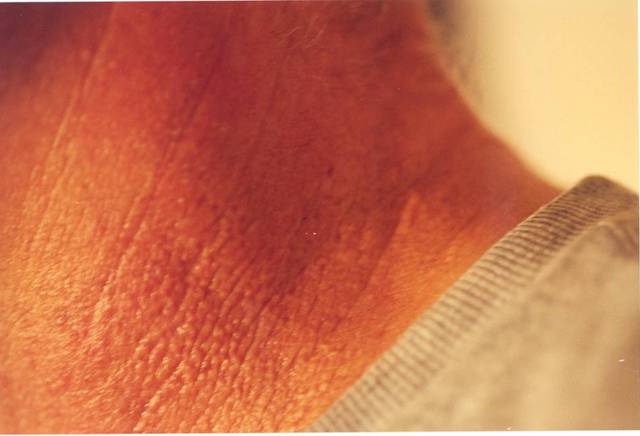
Pilomatricoma is a benign skin neoplasm that can exhibit wide protean manifestations, appearing most commonly as a solitary, deep-seated, firm nodule with a normal to the semi-transparent epidermis. Occasionally, they can be superficial and exhibit a faint red to blue appearance, with deposits of calcium eroded through the skin surface. (1) Graham and Merwin described the “tent sign” as part of the clinical exam to visualize the multifaceted nature of the mass, which is elicited by stretching the skin over the tumor. (2) There are other variants reported including lymphangiectatic, anetodermic and ulcerated. (1) The tumor usually varies in diameter from 0.5 to 3.0 cm, with the largest reported case measuring 20 cm. (3) Pilomatricomas appear most commonly on the head and neck, then upper extremities, and rarely on the trunk or lower extremities. (4) Noguchi et al suggested that the distribution of pilomatricoma corresponds to the density of hair follicles at a particular site. (5) There is a bimodal distribution, in children and adults over 60 years of age, with preponderance in females. (1)
There have been reports of pilomatricomas appearing in association with myotonic dystrophy (6), Gardner’s syndrome (7), and beta-catenin mutations (8). Cases of pilomatricomas associated with hypercalcemia and elevated levels of parathyroid hormone-related protein have also been described. (3)
The histological presentation of pilomatricomas are sharply demarcated, and often surrounded by a connective tissue capsule. They are located in the lower dermis and can extend into the subcutaneous fat. Characteristic features pilomatricomas include irregularly shaped island of epithelial cells embedded in a cellular stroma. These islands contain two main cell populations: 1) basophilic cells that display deeply basophilic nuclei that lie close together and have scanty cytoplasm, and 2) shadow or ghost cells, that have a distinct border and possess a central unstained area as a shadow of the lost nucleus. (9) Calcium deposits are found in approximately 75% of tumors and can be confirmed with the von Kossa stain. (10)
Pilomatricomas are often clinically misdiagnosed, although they are not exceedingly rare, with an incidence rate reported as one of every 500 specimens. (1) Differentials may depend on location, age, and appearance of the nodule. (11) Preoperative diagnoses most commonly include epidermoid cyst, followed by malignancy, inclusion dermoid cyst, and hemangioma. (1)
Fine needle aspiration has been used as a diagnostic tool; however, accurate cytodiagnosis and cytological distinction from other cutaneous lesions, both benign and malignant, remains a challenge. (12) Ultrasonography can be helpful when evaluating tumors in the parotid or breast area. (4) Recurrences, although they do occur (13), are low.
TREATMENT:
Complete surgical excision remains the treatment of choice for benign pilomatricomas.
REFERENCES:
Julian, C. G., & Bowers, P. W. (1998). A clinical review of 209 pilomatricomas. Journal of the American Academy of Dermatology, 39(2 Pt 1), 191-195. https://doi.org/10.1016/S0190-9622(98)70032-1 [PMID: 9708284]
Graham, J. L., & Merwin, C. F. (1978). The tent sign of pilomatricoma. Cutis, 22(5), 577-580.
Kambe, Y., Nakano, H., Kaneko, T., Aizu, T., Ikenaga, S., Harada, K., Nakajima, N., Moritsugu, R., & Hanada, K. (2006). Giant pilomatricoma associated with hypercalcaemia and elevated levels of parathyroid hormone-related protein. British Journal of Dermatology, 155, 208-210. https://doi.org/10.1111/j.1365-2133.2006.07235.x [PMID: 16842501]
Pirouzmanesh, A., Reinisch, J. F., Gonzalez-Gomez, I., Smith, E. M., & Meara, J. G. (2003). Pilomatrixoma: A review of 346 cases. Plastic and Reconstructive Surgery, 112(7), 1784-1789. https://doi.org/10.1097/01.PRS.0000098124.15932.9A [PMID: 14662240]
Noguchi, H., Hayashibana, T., & Ono, T. (1995). A statistical study of calcifying epithelioma, focusing on the site of origin. Journal of Dermatology, 22, 24-27. https://doi.org/10.1111/j.1346-8138.1995.tb03562.x [PMID: 7741024]
Harper, P. S. (1972). Calcifying epithelioma of Malherbe: Association with myotonic muscular dystrophy. Archives of Dermatology, 106(1), 41-44. https://doi.org/10.1001/archderm.1972.01680010043006 [PMID: 5061720]
Leppard, B. J., & Bussey, H. J. (1976). Gardner’s syndrome with epidermoid cysts showing features of pilomatrixomas. Clinical and Experimental Dermatology, 1(1), 75-82. https://doi.org/10.1111/j.1365-2230.1976.tb01009.x
Chan, E. F. (2000). Pilomatricomas contain activating mutations in β-catenin. Journal of the American Academy of Dermatology, 43, 701. https://doi.org/10.1067/mjd.2000.107243
Elder, D. E., Elenitsas, R., & Ragsdale, B. D. (1997). Tumors of the epidermal appendages. In D. E. Elder, R. Elenitsas, C. Jaworsky, & B. Johnson Jr. (Eds.), Lever’s Histopathology of the Skin (8th ed., pp. 747-803). Philadelphia: Lippincott-Raven.
Peterson, W. C. Jr., & Hult, A. M. (1964). Calcifying epithelioma of Malherbe. Archives of Dermatology, 90, 404.
Macleod, A. J., & Scobie, W. G. (1991). Pilomatrixoma as a diagnostic problem: The Edinburgh experience. Journal of the Royal College of Surgeons of Edinburgh, 36(4), 261-263.
Wang, J., Cobb, C. J., Martin, S. E., Venegas, R., Wu, N., & Greaves, T. S. (2002). Pilomatrixoma: Clinicopathologic study of 51 cases with emphasis on cytologic features. Diagnostic Cytopathology, 27, 167-172. https://doi.org/10.1002/dc.10102 [PMID: 12203861]
Aslan, G., Erdogan, B., Aköz, T., Görgü, M., Seçkin, S., & Terzioglu, A. (1996). Multiple occurrence of pilomatrixoma. Plastic and Reconstructive Surgery, 98(3), 510-513. https://doi.org/10.1097/00006534-199609000-00011 [PMID: 8788632]