CORRECT DIAGNOSIS:
Necrobiotic Xanthogranuloma
DISCUSSION:
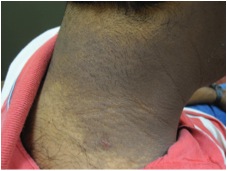
Necrobiotic Xanthogranuloma (NXG) is a relatively rare and chronic granulomatous disease with cutaneous lesions consisting of papules, nodules, or plaques. The lesions tend to have a red to yellow xanthomatous appearance with induration, telangiectasias, and the potential for ulceration, tenderness, pain, and pruritus.1 Typically the lesions are found on the face, specifically the lower and upper eyelids but also have been reported to involve the orbit.1, 2, 4 Other reports state that the lesions can and have initially begun on the trunk and involve internal organs.3 Extracutaneous sites include the respiratory tract, lung, heart, spleen, skeletal muscle, kidney, ovary, and gastrointestinal tract.1,2,3 Our patient had no orbital involvement at the time of presentation.
NXG has a strong association with a paraproteinemia, also referred to as a serum monoclonal gammopathy, involving the IgG K type which occurs in about 80% of the cases.3, 5, 6 Paraproteinemia occurs when increased amounts of a single monoclonal gammaglobulin can be found in the blood. A gammaglobulin is a specific protein fraction of the blood. Other lymphoproliferative and hematologic disorders described with NXG include myeloma and cryoglobulinemia.1, 3, 5 No serum abnormalities were found on initial screening. Abnormalities may arise before or after the onset of skin findings so the patient was referred to hematology and oncology.2
NXG is a rare granulomatous condition that often occurs with a paraproteinemia. All patients need to be screened and closely monitored for cutaneous as well as systemic disease. The patient is currently disease-free and is being followed routinely by dermatology, internal medicine, and hematology and oncology due to the high risk of paraproteinemia.
TREATMENT:
Treatment of NXG mainly focuses on the paraproteinemia, alkylating agents such as chlorambucil, cyclophosphamide, and melphalan have had varied results.1 Topical corticosteroids lack efficacy but intralesional and systemic corticosteroids have had some benefit.2 Systemic steroids in combination with alkylating agents have also been used with varying degrees of success. Wide excision of lesions is not recommended due to the high chance of recurrence. There are reports in the literature of successful treatment of periorbital lesions with excision, but they fail to comment on the length of clearance.2 Current monitoring of the biopsy sites reveal well healing scars with no signs of recurrence in our patient.
REFERENCES:
Mehregan, D. A., & Winkelmann, R. K. (1992). Necrobiotic xanthogranuloma. Archives of Dermatology, 128(1), 94-100. PMID: 1724938
Spicknall, K. E., & Mehregan, D. A. (2009). Necrobiotic xanthogranuloma. International Journal of Dermatology, 48(1), 1-10. PMID: 19187247
Wood, A. J., Wagner, M. V. U., Abbott, J. J., & Gibson, L. E. (2009). Necrobiotic xanthogranuloma: A review of 17 cases with emphasis on clinical and pathologic correlation. Archives of Dermatology, 145(3), 279-284. PMID: 19255321
Stork, J., Kodetova, D., Vosmik, F., & Krejca, M. (2000). Necrobiotic xanthogranuloma presenting as a solitary tumor. The American Journal of Dermatopathology, 22(5), 453-456. PMID: 10932809
Al-Niaimi, F. A., Dawn, G., & Cox, N. H. (2009). Necrobiotic xanthogranuloma without paraproteinaemia: Marked improvement with psoralen ultraviolet A treatment. Clinical and Experimental Dermatology, 35(3), 275-277. PMID: 19364181
Hawryluk, E. B., Izikson, L., & English III, J. C. (2010). Non-infectious granulomatous diseases of the skin and their associated systemic diseases: An evidence-based update to important clinical questions. American Journal of Clinical Dermatology, 11(3), 175-176. PMID: 20425186