Presenter: Nathan Jackson DO, Brittany Carter DO
Dermatology Program: Tri-County Dermatology
Program Director: Dr. Schield Wikas
Submitted on: November 4, 2013
CHIEF COMPLAINT: New onset rash on the legs and feet x 4 days
CLINICAL HISTORY: A 45 year-old Caucasian Female presented with complaint of new onset rash on the legs and feet of 4 days duration. Patient notes initially lesions started as red bumps on the bilateral lower extremities and then developed into “blisters” that had prominent pruritus and burning component. These lesions were painful and accompanied by noticeable swelling. She does feel she had “hives” one week prior to the rash. This was her initial assessment. Medical history included an essential tremor for which she has taken Propranolol for several years. Surgical history included a cholecystectomy, Caesarean section x 2, hysterectomy and tubal ligation (was non-contributory). She has an allergy to latex for which she has not had recent exposure. Most recent events were a “spider bite” two to three weeks prior at which she did not seek treatment. She has no recent infections, exposures to new drugs or chemicals, or other ROS such as arthritis, arthralgias, or systemic involvement except as listed above.
PHYSICAL EXAM:
A full skin exam revealed several non-blanchable, erythematous, ill-defined annular macules and papules on the bilateral distal lower extremities with associated secondary features of serosanguinous filled central bulla. +1/4 non-pitting edema was present bilaterally.


LABORATORY TESTS:
CBC: Leukocytosis, WBC 17.1 with 86% neutrophils on 8/22/2013; resolved on repeat CBC on 9/12/2013
CMP: Gapped metabolic acidosis with CO2 16, resolved on repeat CMP on 9/12/2013
ESR: 19
CRP: 3.6
ANA: negative
Anti-double stranded DNA: <1<0<0<9<3<9
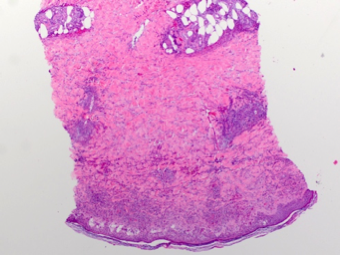
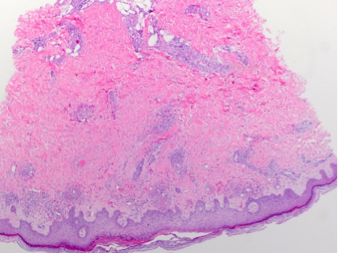
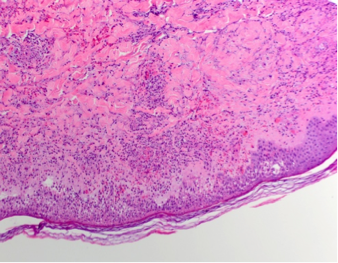
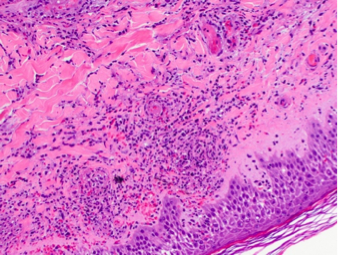
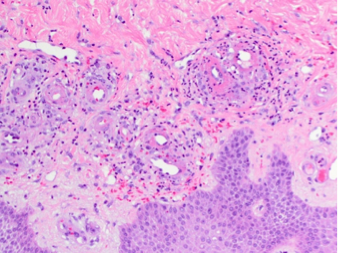
DERMATOHISTOPATHOLOGY:
Punch biopsy sections of the left lower leg demonstrate a reactive epidermis with incipient necrosis including infiltration by the underlying neutrophils. Within the dermis is a brisk superficial and deep perivascular and focally interstitial neutrophilic infiltrate with prominent leukocytoclastic debris. The blood vessels are damaged with fibrinonecrosis of their walls associate with prominent extravasation of erythrocytes. There is no fat necrosis. No evidence of Sweet’s syndrome or large vessel vasculitis. DIF is negative for IgG, IgM, IgA, C3, and fibrinogen.
DIFFERENTIAL DIAGNOSIS:
1. Adverse drug eruption-associated vasculitis
2. Infection
3. Immune Thrombocytopenia Purpura
4. Henoch-Schönlein purpura
5. Cryoglobulinemia




