CORRECT DIAGNOSIS:
Scleredema
DISCUSSION:
Scleredema, originally described by Buschke in 1902, is an uncommon fibromucinous connective tissue disorder characterized by symmetrical diffuse induration of the skin due to accumulation of collagen and aminoglycans in the dermis [1]. Cardiac and other organ involvement is rare, but in severe cases, patients may present with restrictive lung disease [2-3].
Classically, three variants have been described. Type 1 typically affects middle-aged women and is often preceded by acute febrile disease, most commonly of streptococcus origin. A sudden onset hardening of the skin of the cervicofacial region with spontaneous resolution in a period of months to years is seen. Type 2 scleredema appears in individuals without diabetes or infection. This type occurs in women and has an insidious and prolonged course. Monoclonal gammopathy, most commonly IgG, with progression to multiple myeloma may be seen [4-5].
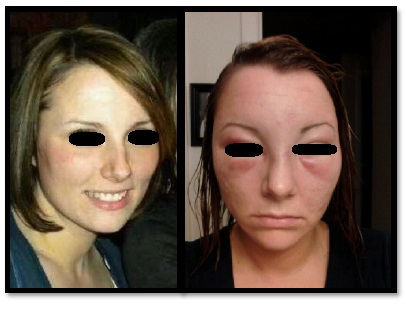
Type 3 occurs primarily in obese, middle-aged men with a long history of insulin-dependent diabetes mellitus, as is the case with our patient [2]. Onset is insidious and induration of the skin of the posterior neck, back, shoulders, and, less commonly, arms is seen [2]. Erythema and a peau d’orange appearance is sometimes present. This third type may be referred to as scleredema diabeticorum. Individuals often have a long history of poor metabolic control as well as diabetic complications; however, cases of scleredema diabeticorum in diabetics with controlled glucose have been reported [6].
The pathogenesis of scleredema diabeticorum is uncertain. Various etiologies have been proposed including irreversible glycosylation of collagen and resistance to degradation by collagenase thus leading to collagen accumulation [7]. Another hypothesis suggests microvascular damage and hypoxia stimulates mucin and collagen synthesis [8].
Diagnosis of scleredema is based on clinical findings of nonpitting, induration or stiffness of the skin, which may be of sudden or insidious onset. Histopathologic confirmation is usually not required. On skin biopsy, the epidermis is usually spared. Thickened collagen bundles within the reticular dermis separated by mucin-containing fenestrations is characteristic. No increase in the number of fibroblasts is seen.
Scleredema may be confused with scleroderma, but the absence of a history of Raynaud’s phenomenon, calcification, or telangiectasia points to scleredema. Scleromyxedema, a generalized primary cutaneous mucinosis that also may have associated monoclonal gammopathy, can be differentiated from scleredema by the diffuse, waxy papules, often in a linear array, in addition to the proliferation of fibroblasts seen histologically.
TREATMENT:
Scleredema diabeticorum often follows an indolent course and unfortunately, lesions may persist, despite good metabolic control. For most patients, it is a relatively mild disorder, although rarely death may occur when internal organs are involved [9]. Multiple treatment modalities have been reported with variable success including corticosteroids, cyclosporine [10], methotrexate [11], electron beam radiotherapy [3], and tamoxifen [12]. More recently, ultraviolet A-1 phototherapy and psoralen with ultraviolet A has been effective in patients with scleredema diabeticorum [6]. Our patient was asymptomatic and opted close follow-up.
REFERENCES:
Buschke, A. (1902). Ueber scleroderma. Klinische Wochenschrift, 39, 955-957. https://doi.org/10.1007/BF01774067
Venencie, P., Powell, F., Su, W., & Perry, H. (1984). Scleredema: A review of thirty-three cases. Journal of the American Academy of Dermatology, 11, 128-134. https://doi.org/10.1016/S0190-9622(84)70104-7
Tamburin, L., & Pena, J. (1998). Scleredema of Buschke successfully treated with electron beam therapy. JAMA Archives of Dermatology, 134, 419-422. https://doi.org/10.1001/archderm.134.4.419
Salisbury, J. A., Shallcross, H., & Leigh, I. M. (1988). Scleredema of Buschke associated with multiple myeloma. Clinical and Experimental Dermatology, 13, 269-270. https://doi.org/10.1111/j.1365-2230.1988.tb01563.x
Kovary, P., Vakilzadeh, F., Macher, E., Zaun, H., Merk, H., & Goerz, G. (1981). Monoclonal gammopathy in scleredema: Observations in three cases. Archives of Dermatology, 117, 536-539. https://doi.org/10.1001/archderm.117.8.536
Martin, C., Requena, L., Manrique, K., Manzarbeitia, F., & Rovira, A. (2011). Scleredema diabeticorum in a patient with type 2 diabetes mellitus. Case Reports in Endocrinology. https://doi.org/10.1155/2011/908452
Graff, R. (1968). Discussion of scleredema adultorum. Archives of Dermatology, 14, 1-18.
Koga, N. (2001). Effects of low-density lipoprotein apheresis on coronary and carotid atherosclerosis and diabetic scleredema in patients with severe hypercholesterolemia. Therapeutic Apheresis, 5(4), 244-251. https://doi.org/10.1046/j.1526-0968.2001.00036.x
Curtis, A. C., & Shulak, B. M. (1965). Scleredema adultorum: Not always a benign self-limited disease. Archives of Dermatology, 92, 526-541. https://doi.org/10.1001/archderm.1965.01600020044004
Mattheou-Vakali, G., Ioannides, D., Thomas, T., Lazaridou, E., Tsogas, P., & Minas, A. (1996). Cyclosporine in scleredema. Journal of the American Academy of Dermatology, 35, 990-991. https://doi.org/10.1016/S0190-9622(96)90077-1
Breuckmann, F., Appelhans, C., Harati, A., Rotterdam, S., Altmeyer, P., & Kreuter, A. (2005). Failure of low-dose methotrexate in the treatment of scleredema diabeticorum in seven cases. Dermatology, 211, 299-301. https://doi.org/10.1159/000087828
Alsaeedi, S., & Lee, P. (2010). Treatment of scleredema diabeticorum with tamoxifen. The Journal of Rheumatology, 37, 2636-2637. https://doi.org/10.3899/jrheum.100193