CORRECT DIAGNOSIS:
Epidermolysis Bullosa Simplex: Localized (Weber-Cockayne)
DISCUSSION:
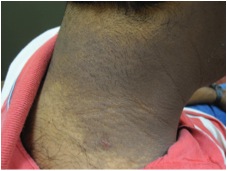
Epidermolysis bullosa simplex (EBS) is a group of hereditary epidermolysis bullosa (HEB) disorders characterized by skin fragility resulting in intraepidermal blisters and erosions that occur either spontaneously or after physical trauma. Reported prevalence ranges from 1/215,000 in the USA to 1/35,000 in Scotland. Onset is usually at or shortly after birth, although blistering in localized EBS may not develop until late childhood or early adulthood. Along with localized or generalized blistering and erosions, sometimes showing characteristic patterns (herpetiform grouping), cutaneous features may include nail shedding and dystrophy, and, rarely, milia formation. Scarring is mostly absent or minimal (mild atrophic wrinkling and dyspigmentation). Other findings may include congenital absence of the skin and localized or confluent keratoderma of the palms and soles.
The commonest extracutaneous manifestation is the blistering of the oral cavity. A variety of additional extracutaneous complications may occur and are age-dependent, with a time of onset and cumulative risk of occurrence highly dependent on the EB subtype. Several subtypes exist based on the intraepidermal localization of blisters. In most, blisters occur in the basal layer of the epidermis. However, 3 subtypes involve suprabasal blistering. EBS is caused by genetic mutations in specific genes depending on the subtype. Diagnosis is based on the determination of the epidermal level within which blisters develop following minor skin traction.
In this case, the patient demonstrated the localized variant, formerly referred to as Weber-Cockayne subtype. The inheritance for this subtype is autosomal dominant with defective proteins keratin 5 and 14. This subtype is characterized by acral bullae at sites of traction or friction . Recommended diagnostic techniques are immunofluorescence antigen mapping (IFM) and transmission electron microscopy (TEM) performed on a skin biopsy sample. Subtypes are then defined on the basis of the mode of transmission, IFM and TEM, and clinical presentation.
Diagnosis is usually straightforward with little need for extensive differential diagnosis. However, in the neonatal period, in utero herpes simplex infection may be considered, especially if there is no family history of a blistering disease or if clinical findings are atypical for EB. The differential diagnosis in neonates and small children may include congenital aplasia cutis, neonatal pemphigus, neonatal herpes gestationis, staphylococcal scalded skin syndrome, as well as incontinentia pigmenti, epidermolytic ichthyosis, linear IgA dermatosis, bullous pemphigoid, and bullous impetigo. Inheritance is either autosomal dominant or autosomal recessive, depending on the subtype. The correct diagnosis of EBS subtype is crucial to proper genetic counseling.
Management is based on the avoidance of blistering by meticulous protective skin padding and appropriate lifestyle to avoid trauma, as well as prevention of secondary infection by careful wound care. Botox injections can repress the hyperhidrosis that exacerbates blistering and nerve blocks are options for refractory, painful cases. Air-conditioning may help in preventing disease worsening in warm weather. Prognosis is highly variable and dependent on the subtype. Most patients have a normal life expectancy but significant morbidity and even early death may occur in some subtypes.
TREATMENT:
Preventative and symptomatic care was initiated. Treatment options discussed included Drysol, Robinul, Botox injections, and ionophoresis (Drionic). Recommendations were given to decrease high impact activities and to limit the amount that feet sweat in general. The patient opted for Drysol Dab-O-Matic 20% topical solution for daily use. Three weeks later at follow-up, she reported some improvement, even given some inconsistency in usage and wished to continue treatment course. We will continue to follow her for improvement, instituting Botox injections for hyperhidrosis, and possible nerve block as a secondary option if Drysol treatment fails.

REFERENCES: