CORRECT DIAGNOSIS:
Pityriasis Rubra Pilaris
DISCUSSION:
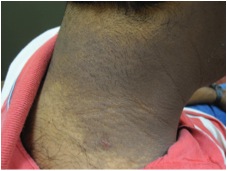
Pityriasis Rubra Pilaris (PRP) is an uncommon, chronic skin condition of unknown etiology. It is characterized by hyperkeratotic follicular papules and palmoplantar keratoderma. The coalescence of papules bordered by uninvolved skin creates the appearance of “islands of sparing” between salmon-colored, scaling plaques. The progression of erythroderma is a potential complication. PRP affects approximately 2.5 per million of the population and does not differ based on race or gender. There is a bimodal distribution for the age of onset, including childhood for familial cases and the fifth or sixth decade for acquired cases1,2.
The Griffiths’ classification scheme describes six different types of PRP, differing in clinical presentation, lesion distribution, course, and duration. The majority of patients are Type I, “classic adult,” with generalized distribution and a cephalocaudal progression. In addition to the cosmetic and functional implications of the tight scales of the scalp and face, the waxy, thickened skin of the soles, and palms can crack resulting in painful fissures. The onset is acute and 80% resolve within a three year period3.
While the pathogenesis of PRP remains uncertain, abnormal vitamin A metabolism, specifically a deficiency of retinol-binding protein, and human immunodeficiency virus (HIV) have been studied as possible causes. Autoimmune diseases, infections, and malignancies are linked as trigger factors; however, most cases occur without an inciting event4. The familial type of PRP, Type V, follows an autosomal dominant mode of inheritance, early age of onset, incomplete penetrance, and variable expression. In a recent study, Fuchs-Telem et. al. showed that mutations in CARD14, which regulates inflammatory processes through nuclear factor kappa B (NF-kB) and is strongly expressed in the skin, cause familial PRP5.
There is no universally effective treatment for PRP and some cases may even demonstrate resistance to both systemic and topical therapies6. A lack of thorough research comparing current treatment options exists due to the rarity of the condition. Traditionally, retinoids and methotrexate are used as systemic therapy. Topical emollients, corticosteroids, and keratolytics supplement the oral treatment. Biologic medications against psoriasis, such as tumor necrosis factor (TNF) antagonists, may have value in treating PRP, given the histological and clinical similarities between the two diseases4,7.
TREATMENT:
At the initial visit, the patient was started on triamcinolone cream and instructed to follow up in two days to review his biopsy results. Initial follow-up revealed progressing erythroderma in a cephalad to caudad direction with areas of uninvolved skin as well as more extensive hyperkeratosis of the palms and soles with fissuring. At this time, he was started on oral cyclosporine and acitretin. Despite these medications, the erythroderma progressed and he developed 3+ pitting edema of the lower extremities. He was admitted to the hospital for fluid and electrolyte management. During the hospitalization, his laboratory abnormalities included mild hypoalbuminemia and hypoproteinemia. Following hospital discharge, the patient’s dose of cyclosporine has been progressively tapered, and the dose of acitretin has been increased. The patient remains erythrodermic but has experienced much less scaling, and the fissuring to his palms and soles has resolved. He continues to experience moderate pruritus and difficulty in body temperature regulation.
REFERENCES:
1. Griffiths A. Pityriasis Rubra Pilaris. Dowling Oration. 2003. URL http://www.prp-support.org/wp/wp-content/uploads/2014/03/Griffiths-Dowling-Oration-2003.pdfpdf (last accessed: 9 September 2014).
2. Griffiths WA. Pityriasis Rubra Pilaris – An Historical Approach. 2. Clinical features. Clin Exp Dermatol. 1976; 1: 37–50.
3. Griffiths WAD. Pityriasis Rubra Pilaris. Clin Exp Dermatol. 5:105, 1980
4. Klein A, Landthaler M, Karrer S. “Pityriasis Rubra Pilaris: A Review of Diagnosis and Treatment.” Am J Clin Dermatol. 2010; 11:157-70
5. Fuchs-Telem D, Sarig O, Van Steensel M et al. Familial Pityriasis Rubra Pilaris Is Caused by Mutations in CARD14. Am J Hum Genet. 2012; 91:163-70.
6. Müller H, Gattringer C, Zelger B et al. Infliximab Monotherapy as First-line Treatment for Adult-onset Pityriasis Rubra Pilaris: Case Report and Review of the Literature on Biologic Therapy. J Am Acad Dermatol. 2008; 58: S65-70.
7. Ivanova K, Itin P, Haeusermann P. Pityriasis Rubra Pilaris: Treatment with Biologics – A New Promising Therapy? Dermatol. 2012;224: 120-25