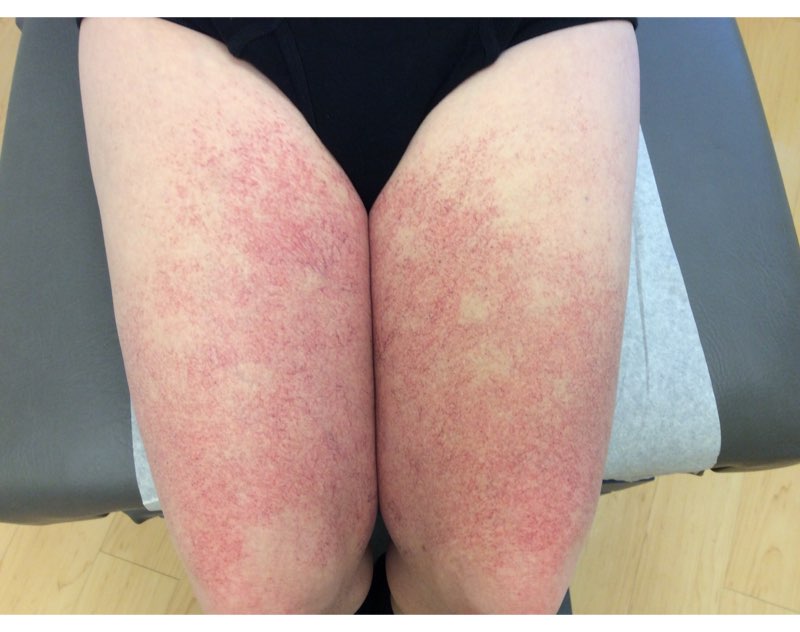
CORRECT DIAGNOSIS:
Pityriasis lichenoides chronica
DISCUSSION:
Pityriasis lichenoides chronica (PLC) exists on a spectrum with pityriasis lichenoides et varioliformis actua (PLEVA). Both are characterized by recurrent crops of spontaneously regressing lesions and are due to a clonal T-cell proliferation with a predominance of CD8+ cells in PLEVA and a predominance of CD4+ cells in PLC. The cause of this clonal proliferation is unknown but infectious etiologies and drugs have been suspected in some cases. An abundance of maternally derived keratinocytes in lesional skin when compared to non-lesional skin has also been noted in some male patients and speculation has been made that this may be a reaction similar to a host versus graft reaction.
The clinical features of the rash vary between PLEVA and PLC. PLEVA lesions are typically vesicular or pustular while PLC lesions are scaly. The lesions are often asymptomatic. Pityriasis lichenoides is more often seen in the pediatric population with a slight male predominance. One study demonstrated that the distribution of the rash is a more important factor in determining prognosis than the appearance of the lesions. The average time to spontaneous clearance was seen at 11 months for diffuse involvement compared to 33 months when the distribution was primarily peripheral.
Typical histopathology findings include a superficial perivascular vacuolar interface dermatitis with lymphocytes predominant in the infiltrate. Within the vacuolar interface, there is a lymphocyte in nearly every vacuole. Transepidermal extravasation of erythrocytes is often seen. The eosinophils mentioned in the dermatohistopathology section are not a typical feature of PLC; however, these were rare and the dermatopathologist reading the slide still favored the diagnosis of pityriasis lichenoides since it correlated well clinically.
TREATMENT:
As noted previously, the oral steroid taper nearly resolved the rash; however, it returned once they were discontinued. Currently, patient is taking oral erythromycin and has experienced slow, progressive improvement of rash.
REFERENCES:
Bolognia, J.L., Jorizzo, J.L., & Schaffer, J.V. (2012). Dermatology (3rd ed., pp. 159-161). Spain: Elsevier.
Muhlbauer, J.E., Bhan, A.K., Harrist, T.J., et al. (1984). Immunopathology of pityriasis lichenoides acuta. Journal of the American Academy of Dermatology, 10, 783-795.
Elston, D.M., & Ferringer, T. (2014). Dermatopathology (2nd ed., p. 141). N.p.: Saunders Elsevier.
Glemetti, C., Rigoni, C., Alessi, E., et al. (1990). Pityriasis lichenoides in children: A long-term follow-up of eighty-nine cases. Journal of the American Academy of Dermatology, 23, 473-478.