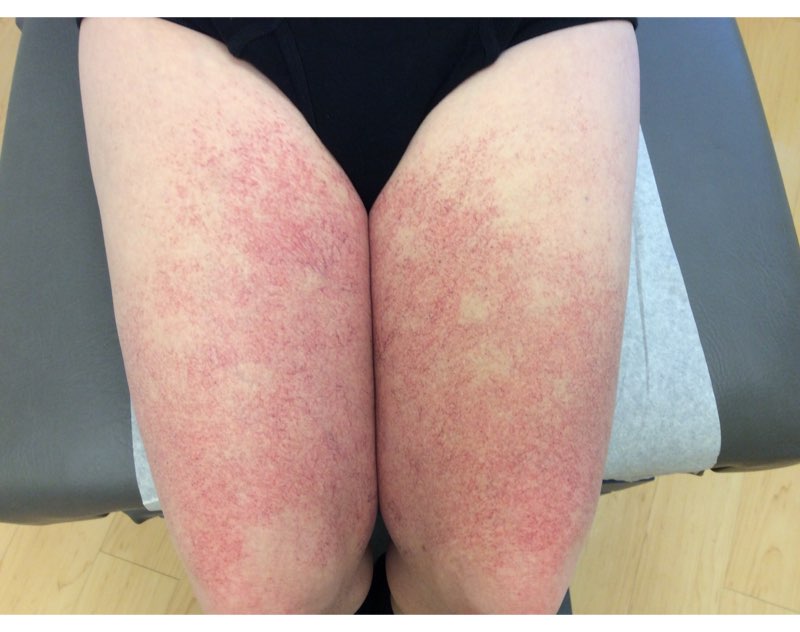
CORRECT DIAGNOSIS:
TNF-alpha Inhibitor-induced Psoriasis
DISCUSSION:
The development of psoriasiform lesions in patients undergoing TNF-alpha inhibitor therapy has an incidence as high as 5%, with pustular psoriasis being the most common presentation. The current TNF-alpha inhibitors on the market and reported causing this adverse event are infliximab, etanercept, and adalimumab. Patients frequently present with more than one form of induced psoriasis, but nail psoriasis is far less reported. Noted nail findings are onycholysis, onychodystrophy, “oil-spotting,” subungal hyperkeratosis, and discoloration. While there is no proven predilection, it has been suggested through a literature review that up to 70% of patients who develop this class effect are female. While patients with a personal or familial history of inflammatory skin lesions may be at an increased risk of developing paradoxical psoriasis, 87% in one review reported de novo development of the psoriatic lesions following the use of TNF-alpha inhibitors (2). The etiology is still unknown but believed to be caused by multiple factors and possibly pre-determined risk factors in the patient.
TREATMENT:
Treatment is the cessation of TNF-alpha inhibitor therapy, as discussed with the prescribing physician, and as tolerated by the patient. Some patients have been known to tolerate continued TNF-alpha inhibitor treatment with adjuvant anti-psoriatic treatment. The addition of corticosteroids, keratolytics, vitamin D analogs, methotrexate, cyclosporine, and phototherapy have all been discussed as successful treatment options.
Our patient was started on topical therapy using calcipotriene 0.005% cream daily and triamcinolone acetonide 0.1% cream twice daily to the anal area, as well as extremities. Upon an interdisciplinary discussion with the patient’s gastroenterologist, infliximab was stopped and she was subsequently started on weekly subcutaneous Methotrexate 10mg and Prednisone 15 mg daily to control her UC. At one month follow up, there was a great improvement in her skin lesions but no change in nail psoriasis. She was then started on phototherapy using the 308 nm Excimer Laser with a starting dose of 400 mJ/cm2 as well as Apremilast 30 mg twice daily.
REFERENCES:
Rahier JF, Buche S, et al. Severe Skin Lesions Cause Patients with Inflammatory Bowel Disease to Discontinue Anti-TNF Therapy. Clin Gastroenterol H. 2010; 8 (12):1048-1055.
Puig L, Morales-Munera CE, et al. Ustekinumab Treatment of TNF Antagonist-Induced Paradoxical Psoriasis Flare in a Patient with Psoriatic Arthritis: Case Report and Review. Dermatology. 2012; 225:14-17.
Collamer AN, Guerrero KT, et al. Psoriatic skin lesions induced by tumor necrosis factor antagonist therapy: A literature review and potential mechanisms of action. Arthritis Rheum. 2008; 59: 996–1001.
Wollina U, Hansel G, et al. Tumor Necrosis Factor-a Inhibitor-Induced Psoriasis or Psoiasiform Exanthemata. Am J Clin Dermatol. 2008; 9(1):1-14.
Sfikakis PP, Iliopoulos A, et al. Psoriasis induced by anti–tumor necrosis factor therapy: A paradoxical adverse reaction. Arthritis Rheum. 2005; 52: 2513–2518.
Moustou AE, et al. Cutaneous side effects of anti-tumor necrosis factor biologic therapy: A clinical review. J Am Acad Dermatol. 2009; 61(3): 486-504.