Presenter: John Howard, DO
Dermatology Program: Larkin Community Hospital/NSU-COM, South Miami, FL
Program Director: Stanley Skopit, DO, MSE, FAOCD, FAAD
Submitted on: October 26, 2016
CHIEF COMPLAINT: progressively worsening pruritic rash on her extremities and trunk
CLINICAL HISTORY: A 12-year-old African American female with a history of immunodeficiency syndrome due to an NF-kappa-B essential modulator (NEMO) gene mutation, currently status post umbilical CBT before age 1 with myeloablation-induced hypothyroidism and hypoestrogenism, presented to Advanced Dermatology & Cosmetic Surgery in Margate, Florida as an outpatient complaining of a progressively worsening, pruritic, hypertrophic, and lichenified plaques and papules on truck and extremities for several months. The patient denies preceding or current upper respiratory infection, cough, sore throat, fever, chills, arthralgias, or diarrhea. She presents with recent negative bloodwork for South Florida environment allergy panel and negative T.R.U.E. allergy patch testing. Her only medications are levothyroxine 62.5mcg daily and estradiol 0.025 mg/hr weekly patch for Hashimoto thyroiditis-induced hypothyroidism and hypoestrogenism respectively. She has no known drug allergies. Family history is significant for an older brother who unfortunately passed away shortly after birth due to a NEMO mutation and the mother states she is the carrier. Patient has been using mild-potency topical steroid creams and oils and lotions.
Incidentally, her mother was noted to have dark brown hyperpigmented thin plaques in a blaschkoid distribution on bilateral posterior lower extremities. The mother refused a skin biopsy, which was explained could support the clinical impression of IP. Taken in total, mother and daughter share a mutation in NEMO, however, the mother’s phenotype is that of IP and the daughter’s phenotype that of anhidrotic ectodermal dysplasia with immunodeficiency (AED-ID).
PHYSICAL EXAM:
Physical exam revealed monomorphic well-demarcated thick silvery-white scaly erythematous plaques throughout arms, legs, and trunk affecting 15% of her total body surface area. Nails showed irregular pitting. Palms and scalp were not affected however plantar feet were scaly.
Digits were non-tender and non-edematous. No mucous membrane abnormalities were observed. Sparse dentition noted with few widely spaced teeth and braces present.


LABORATORY TESTS:
Bloodwork was negative or within normal limits for complete blood count with differential, a complete metabolic panel including liver function studies, thyroid stimulating hormone, follicle stimulating hormone, luteinizing hormone, quantiferon gold, and chronic hepatitis panel.
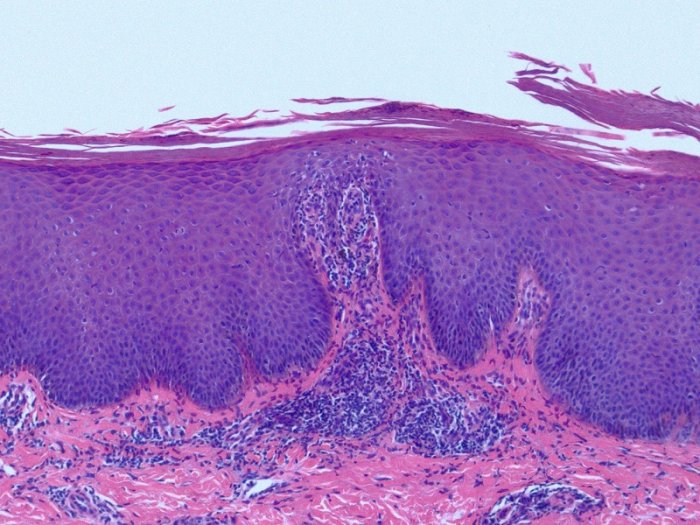
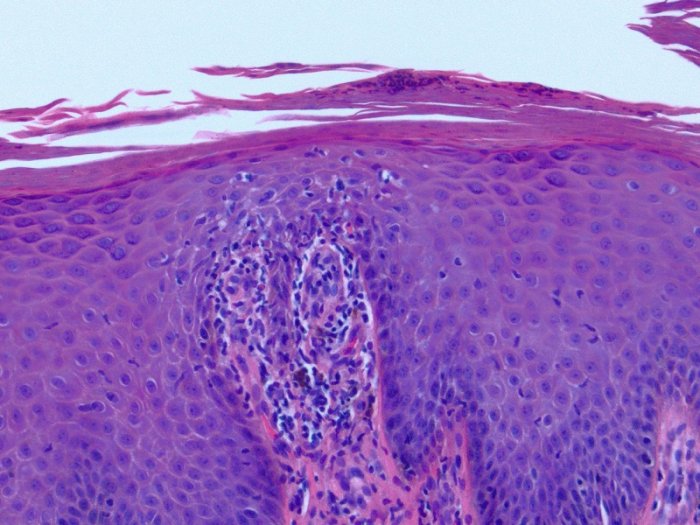
DERMATOHISTOPATHOLOGY:
A 3mm punch biopsy of a plaque from the left thigh showed neutrophils in the stratum corneum, thinning of suprapapillary plates, regular epidermal acanthosis, and hypogranulosis consistent with psoriasis. Two additional punch biopsies at the left posterior arm and right upper back were performed 8 weeks later, for a more thorough check to rule out possible graft-versus-host disease, were both consistent with plaque psoriasis.
DIFFERENTIAL DIAGNOSIS:
1. Chronic Plaque Psoriasis
2. Hypertrophic Lichen Planus
3. Graft-versus-host disease
4. Contact Dermatitis
5. Atopic Dermatitis




