Presenter: Michelle Elway DO, George Brant DO, Jonathan Bielfield DO
Dermatology Program: Colorado Dermatology Institute, RVU
Program Director: Reagan Anderson DO
Submitted on: November 29, 2016
CHIEF COMPLAINT: Diffuse rash
CLINICAL HISTORY: A 44-year-old Burmese female with no significant past medical history presented with fever, pain, swelling, and erythema of her right thumb after a closed injury while working with raw chicken at work. She was diagnosed with a felon and a P1 fracture, subsequently undergoing an I&D. She was then placed on vancomycin, ceftriaxone, and metronidazole for possible exposure to raw chicken to cover empirically for enteric bacteria (salmonella, E. coli, Enterococcus) as well as for skin flora with negative cultures. While being evaluated by ID, they noted multiple dry, erythematous plaques on the face and extremities. They determined “it was likely rheumatologic”, as the patient reported it being present since 2014, and treated by her PCP in Burma. No further workup was performed on that admission. The patient’s thumb improved, and she was discharged home three days later with a 5-day course of Bactrim and amoxicillin.
Approximately four weeks later, the patient returned to the Emergency Department with facial swelling and a worsening “rash”. The ED thought the rash may be an allergic reaction, SJS, or TEN. Dermatology was then consulted and found a previously healthy female presenting with a worsening diffuse rash reportedly over the previous month. However, prior hospital documentation revealed a history of an ongoing rash since 2014, which was managed by a physician in Burma. The patient also reported living in the United States for six years and works in a chicken processing and packing factory. She denied any sick contacts at home.
Per the patient, the rash started 4 weeks ago on her face and spread down her body after the previous hospitalization. Per the patient’s son, she had been experiencing vomiting and nausea over the past week, which resolved one day prior. The patient also reported a stuffy nose, cough, and hoarse voice. Later, during admission, the patient was followed by ENT due to concerns for the hoarse voice and respiratory compromise. PCP in Burma treated rash on the face with topical cream approximately 6 years ago.
PHYSICAL EXAM:
• Afebrile, NAD
• HEENT: no conjunctival injections, no swelling of the soft palate, no erythema in the posterior pharynx
• Skin: Fitzpatrick III
• Well-demarcated and indurated erythematous to brown plaques with rare overlying scale on the forehead, cheeks, bilateral ears, left breast, right abdomen, upper and lower extremities
• Intact pinprick of upper extremity plaques
• Absent pinprick and temperature sensation in lower extremity plaques
• Necrotic ulceration of left 1st metatarsal without surrounding erythema
• No atrophy of the limbs on examination
Leonine face with granulomatous plaques: 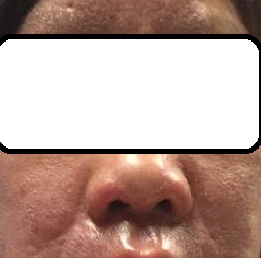


LABORATORY TESTS:
Punch Biopsies performed to indurated plaques of the left medial calf and right brachium
Tissue Cultures sent for aerobic, anaerobic, fungal, and AFB.
Tissue cultures sent for mycobacterium leprosy PCR to Hanson’s registry in Baton Rouge, LA.
Lab tests:
CRP 86.3, ESR 78
DERMATOHISTOPATHOLOGY:
Granulomatous process concerning leprosy showing granulomatous inflammation along cutaneous nerves with identification of organisms on fite stain consistent for leprosy.
DIFFERENTIAL DIAGNOSIS:
1. Leprosy
2. Atypical myobacterial infection
3. Sarcoidosis
4. Deep fungal infection
5. Mycosis fungoides




