CORRECT DIAGNOSIS:
Acute Generalized Exanthematous Pustulosis
DISCUSSION:
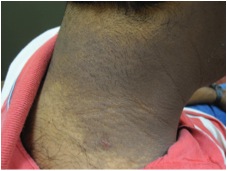
Acute generalized exanthematous pustulosis (AGEP) is an uncommon acute, febrile drug eruption. It is characterized by numerous small, non-follicular sterile pustules that arise on a background of edematous erythema. The lesions generally begin on the face or major intertriginous zones and quickly disseminate over a few hours. Associated symptoms may include burning, pruritus, or both, and edema of the face and hands. Purpura and bullae can be seen in 50% of cases. The eruption typically lasts 1 to 2 weeks and is followed by superficial desquamation that heals without scarring.
The majority of cases are drug-induced, with a small percentage due to viral infections or exposure to mercury. The most frequently implicated drugs include beta-lactam antibiotics and macrolides, followed by calcium channel blocks (specifically diltiazem) and antimalarials. AGEP has also been reported in association with other antimicrobials, including tetracyclines, metronidazole, terbinafine, isoniazid, and vancomycin. AGEP associated with ciprofloxacin has only been reported in two prior cases in the literature. A short interval (< 4 days) between drug administration and the onset of the eruption is characteristic of AGEP and is thought to be due to prior sensitization to the drug that indicates an immunologic recall phenomenon. Patch testing with the incriminated drug is positive in 80% of cases.
While the pathogenesis has not been completely elucidated, drug-specific T-lymphocytes have been found to produce high amounts of neutrophil-attracting chemokines including IL-8. Blood neutrophilia may also be present in patients with AGEP. On histopathologic examination, subcorneal spongiform pustules will be seen, along with edema of the papillary dermis and a mixed infiltrate including neutrophils and eosinophils. Clinically, AGEP can be confused with acute pustular psoriasis, which can be compounded by the fact that AGEP occurs more frequently in patients, like ours, with a history of psoriasis.
TREATMENT:
The mainstay of treatment for AGEP is the withdrawal of the responsible drug. A drug chart can be utilized to identify the most likely incriminating drug. Topical steroids and antipyretics can be used for symptomatic relief. Upon review of EMR records, our patient had a previous history of AGEP just 3 months prior, which was incorrectly attributed to vancomycin. A closer review of the medications started during that admission, in conjunction with the present history, concluded that ciprofloxacin was in fact the culprit drug. Ciprofloxacin was discontinued and she was treated topically with bland emollients. Complete resolution and reepithelialization were achieved within 1-2 weeks.
REFERENCES:
Bolognia JL, Jorizzo JL, Schaffer JV. Dermatology, 3rd Ed. Spain: Elsevier, 2012: 752-754.
Speeckaert MM, Speeckaert R, Lambert J, Brochez L. Acute generalized exanthematous pustulosis: an overview of the clinical, immunological and diagnostic concepts. Eur. J. Dermatol. 2010;20(4):425–433.
Roujeau JC, Bioulac-Sage P, Bourseau C. Acute generalized exanthematous pustulosis. Analysis of 63 cases. Arch. Dermatol. 1991;127(9):1333–1338.
Hausermann P1, Scherer K, Weber M, Bircher AJ. Ciprofloxacin-induced acute generalized exanthematous pustulosis mimicking bullous drug eruption confirmed by a positive patch test. Dermatology. 2005;211(3):277-80.