Presenter: Roxanne Rajaii DO, Derek Hirschman DO, Summer Moon DO, Megan Furniss DO, Nichelle Arnold DO, Bryan Gray DO
Dermatology Program: Botsford Hospital
Program Director: Annette LaCasse DO
Submitted on: March 12, 2017
CHIEF COMPLAINT: Erythematous and mildly pruritic rash on central chest and bilateral breasts.
CLINICAL HISTORY: A 29-year-old Caucasian female presented with chief complaint of an erythematous and mildly pruritic rash localized to bilateral breasts and present for approximately one year. The patient denied any recent infections, new medications, or exacerbating factors. She denied any other constitutional symptoms including but not limited to fever, chills, and night sweats. She did admit to a long-standing history of smoking but stated that she is in the process of cessation. Patient reported exacerbation of skin lesions with sun exposure. Patient had been previously treated with topical combination hydrocortisone and lotramine, as well as topical clotrimazole/betamethasone diproprionate ointments with no improvement.
PHYSICAL EXAM:
On examination, the patient had erythematous reticulated plaques on the lateral aspects of bilateral breasts, with more involvement of the left breast compared to the right. There was also slight erythema with scattered papules in the lower sternal region. She complained of mild pruritus but denied any other associated symptoms. Cutaneous involvement was localized to the areas described above.



LABORATORY TESTS:
The following laboratory assessments were obtained: complete blood count with differential (CBC with diff), aspartate aminotransferase (AST), alanine aminotransferase (ALT), serum blood urea nitrogen (BUN), serum creatinine (CR), human immunodeficiency virus (HIV), antinuclear (ANA) antibody, ribonucleoprotein (anti-U1-RNP) antibody, scleroderma antibody (anti-Scl-70), smith antibody (anti-Sm), and glucose-6-phosphate dehydrogenase (G6PD) testing. All labs were negative or within normal limits, with the exception of a white blood cell count of 19.3 Thous/uL (reference range: 4.0-11.3 Thous/uL) with an absolute neutrophilia of 16.9 Thous/uL (reference range: 1.8-8.0 Thous/uL).
DERMATOHISTOPATHOLOGY:
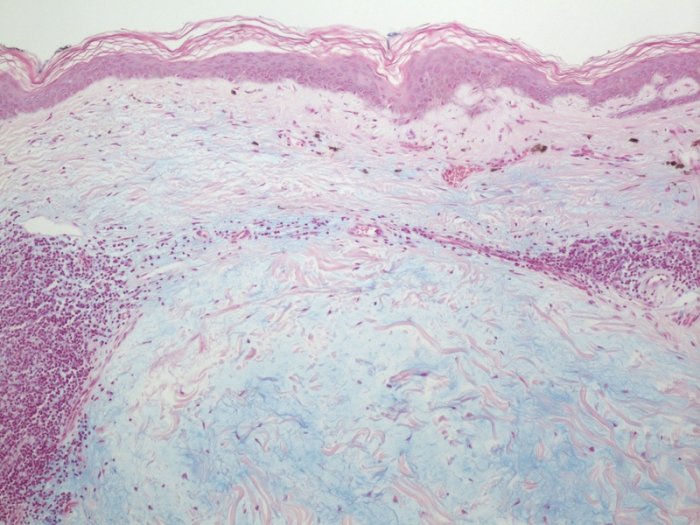
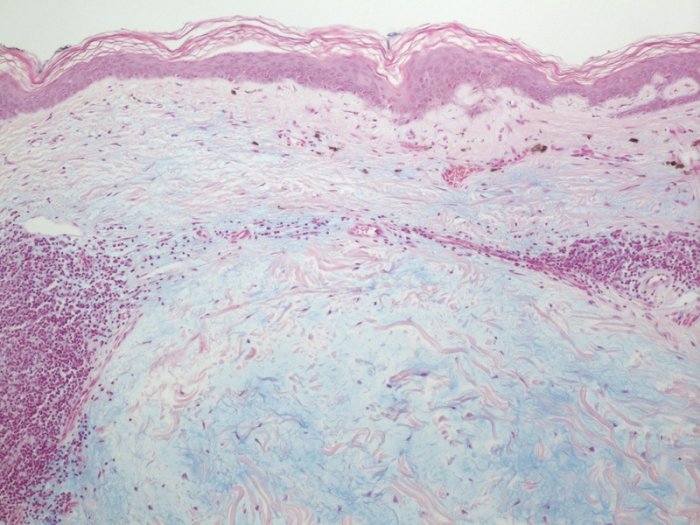
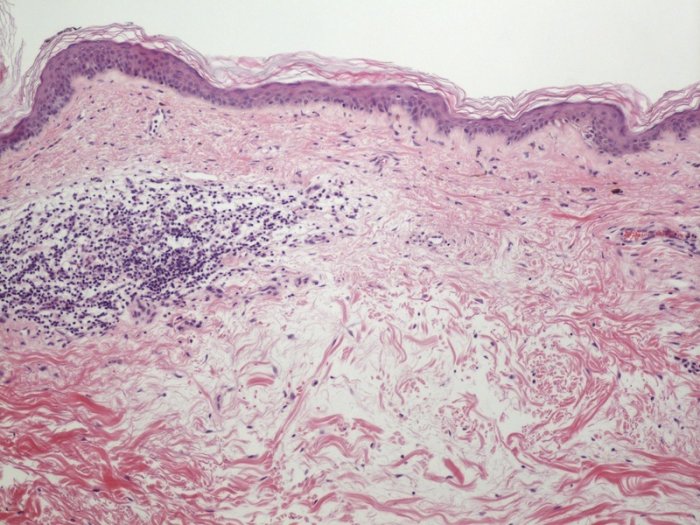
The initial work-up included a 4 mm punch biopsy of the reticulated plaque of the left breast. The biopsy showed a moderately dense superficial to mid perivascular inflammatory cell infiltrate consisting predominantly of lymphocytes. The collagen fibers within the reticular dermis were widely separated, and an Alcian blue stain showed deposition of increased dermal mucin within these spaces .
DIFFERENTIAL DIAGNOSIS:
1. Irritant/Allergic contact dermatitis
2. Tumid Lupus Erythematosus
3. Tinea corporis
4. Interstitial granuloma annulare
5. Reticular erythematous mucinosis