CORRECT DIAGNOSIS:
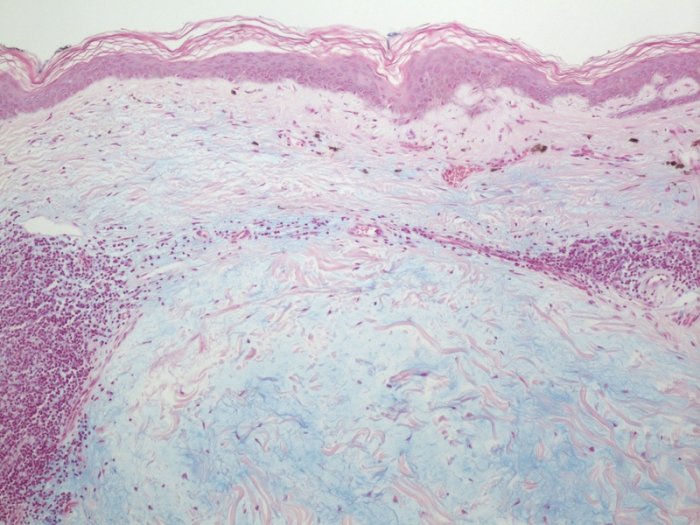
Reticular Erythematous Mucinosis (REM)
DISCUSSION:
Reticular erythematous mucinosis (REM) is a rare skin condition that was initially classified as an entity in 1974, though similar clinical and histological descriptions of plaque-like cutaneous mucinosis date back to 1960. REM typically affects middle-aged females (almost always between 10 and 73 years of age), with a female: male ratio of 2:1. Clinically, remission is common and the hallmark features of this disease are erythematous macules and papules that coalesce into a reticulated pattern, favoring the midline (anteriorly on the central chest or posteriorly on the mid-back). These macules and papules may be indurated but lack scale or other surface changes, and may also be less commonly found on the neck, face, upper abdomen, and limbs. Most patients show no associated clinical symptoms, though 20-30% of patients report pruritus and even less frequently, a slight burning sensation.
Since its initial characterization, REM has been controversially associated with solar irradiation. Some patients with REM report that sun exposure worsens/triggers REM, while others report no association of REM with sun exposure or even improvement of REM symptoms after sun exposure. Smoking appears to be another risk factor associated with REM, as studies have shown up to 91% concurrence rate. REM has also been found to be associated with several medical conditions, including thyroid disease and internal malignancies of the lung, breast, and colon. Other, less substantiated associations with REM include oral contraceptives, ITP, DLE, diabetes mellitus, hypertension, HIV, and monoclonal gammopathy.
Among treatment options for REM, the most studied and first-line therapy is antimalarials, including hydroxychloroquine (5-6 mg/kg body weight; 400 mg max total daily dose) and chloroquine diphosphate (3-4 mg/kg body weight; 250 mg max total daily dose). These drugs can inhibit the release of IL-2 from CD4+ T cells and inhibit major histocompatibility complex (MHC) expression by macrophages. Most patients found resolution of REM symptoms in 1-2 months following anti-malarial therapy, though some patients had disease recurrence with discontinuation of the drug and others had worsening of REM with antimalarials. Common side effects of these medications can include gastrointestinal, neurologic, and irreversible ophthalmologic manifestations and should be closely monitored. While hydroxychloroquine and chloroquine therapy is contraindicated with pre-existing ophthalmologic conditions, there has been one report of successful REM treatment using quinacrine, as quinacrine has no adverse ophthalmologic effects such as retinopathy or corneal deposits.
TREATMENT:
After clearance by an ophthalmologist and the above laboratory evaluations, the patient was started on 200 mg of hydroxychloroquine daily. Appropriate sun protection of the affected area, as well as smoking cessation, were thoroughly discussed with the patient. Common associations of REM with discoid lupus erythematosus (DLE), idiopathic thrombocytopenic purpura (ITP), diabetes mellitus, thyroid disease, and malignancy were also discussed with the patient, who denied any of these comorbidities. She was instructed to follow-up with her primary care physician for further workup of associated conditions and age-appropriate cancer screening.
REFERENCES:
Kreuter A, Scola N, Tigges C, Altmeyer P, Gambichler T. Clinical features and efficacy of antimalarial treatment for reticular erythematous mucinosis: a case series of 11 patients. Arch Dermatol. 2011 Jun;147(6):710-5. doi: 10.1001/archdermatol.2011.12. PubMed PMID: 21339419.
Braddock SW, Davis CS, Davis RB. Reticular erythematous mucinosis and thrombocytopenic purpura. Report of a case and review of the world literature, including plaquelike cutaneous mucinosis. J Am Acad Dermatol. 1988 Nov;19(5 Pt 1):859-68. Review. PubMed PMID: 3056996.
Steigleder GK, Gartmann H, Linker U. REM syndrome: reticular erythematous mucinosis (round-cell erythematosis), a new entity? Br J Dermatol. 1974 Aug;91(2):191-9. PubMed PMID: 4472292.
Rongioletti F, Merlo V, Riva S, Cozzani E, Cinotti E, Ghigliotti G, Parodi A, Kanitakis J. Reticular erythematous mucinosis: a review of patients’ characteristics, associated conditions, therapy and outcome in 25 cases. Br J Dermatol. 2013 Dec;169(6):1207-11. doi: 10.1111/bjd.12577. PubMed PMID: 23937648.
Kucukunal A, Altunay I, Demirci GT, Sarikaya S, Sakiz D. Reticular erythematous mucinosis on the midline of the back. Cutis. 2014 Jun;93(6):294-6. PubMed PMID: 24999640.
Thareja S, Paghdal K, Lien MH, Fenske NA. Reticular erythematous mucinosis–a review. Int J Dermatol. 2012 Aug;51(8):903-9. doi: 10.1111/j.1365-4632.2011.05292.x. Review. PubMed PMID: 22788804.
Haendchen LC, Sabbag DS, Furlani Wde J, de Souza PK, Rotta O. Reticular erythematous mucinosis. Cutis. 2014 Mar;93(3):E21-4. PubMed PMID: 24738106.
McFadden N, Larsen TE. Reticular erythematous mucinosis and photosensitivity: a case study. Photodermatol. 1988 Dec;5(6):270-2. PubMed PMID: 3249684.
Morison WL, Shea CR, Parrish JA. Reticular erythematous mucinosis syndrome. Report of two cases. Arch Dermatol. 1979 Nov;115(11):1340-2. PubMed PMID: 507890.
Susok L, Kreuter A. Complete clearance of reticular erythematous mucinosis with quinacrine monotherapy. Arch Dermatol. 2012 Jun;148(6):768-9. doi: 10.1001/archdermatol.2012.53. PubMed PMID: 22710470.