CORRECT DIAGNOSIS:
Cellular Dermatofibroma
DISCUSSION:
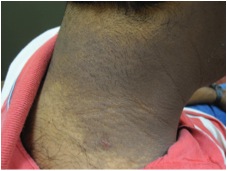
Cellular Dermatofibromas, also known as Cellular Fibrous Histiocytomas are a rare variant of Dermatofibromas and represent only 5% of all cases (1). This variant was first reported by Fukamiza et al in 1983 in the Journal of Cutaneous Pathology under the name “Atypical Pseudosarcomatous Cutaneous Histiocytoma” (2). Epidemiologically, there is a slight male predominance. Clinically these neoplasms are most commonly found on the extremities with slightly more on the upper limb than lower limb and also may be found on the head and neck (3). Tumors can occasionally be found at other areas not typically common for dermatofibromas such as the face, ears, hands, and feet (1). Morphologically there is a polypoid or nodular morphology averaging around 1.5cm in diameter (4). Overall most lesions reportedly had only been present for a few months prior to diagnosis(3).
Histologically these neoplasms are densely cellular with predominantly eosinophilic cytoplasm. There is an infiltrative growth pattern that is fascicular or storiform in appearance, often extending deep into the subcutis. The overlying epidermis often shows variable hyperkeratosis and hyperpigmentation of the basal cell layer. The central area of the neoplasm usually shows the cellular features while lateral edges appear more commonly like typical fibrous histocytomas (1). Immunohistochemical staining (IHC) shows variable SMA positivity, non-neoplastic cell factor XIIIa staining, and variable CD34 staining most commonly at the peripheral margins of the neoplasm (1).
This histological differential includes dermatofibrosarcoma protuberans (DFSP) and leiomyosarcoma. Cellular atypia can be more pronounced in a Cellular Dermatofibroma than in a DFSP in some cases. Immunohistochemical staining does not clearly differentiate this neoplasm compared to a DFSP a known issue to dermatopathologists. Cellular dermatofibromas display a negative Factor XIIIa consistent with a DFSP, but unlike a DFSP staining with Factor CD34 is positive at the lesion edges (5). New IHC approaches with CD163 (positive in cellular dermatofibromas and negative in DFSP) and CD44 have shown promise in use to differentiate these two neoplasm types (6). Leiomyosarcoma shows a more uniform fasicular growth pattern and has a more diffuse SMA and desmin positive staining pattern (1).
A review of the literature for cellular dermatofibromas demonstrates a controversy of whether these neoplasms should be considered malignant or benign. The argument cites the observed high recurrence rate of up to 26% after excision and potential to metastasize as evidence to consider malignant (1, 7). Regardless, tt is recommended that complete excision of these lesion be performed, although no clear guidelines on margin size exists. Aggressive or recurrent lesions may utilize Mohs micrographic surgery for removal, although no specific pathologic findings have been correlated with an increased risk of C. After removal, due to the high risk of recurrence and metastasis it is recommended that close follow-up be performed (6). On average recurrence has been reported to occur with a mean of 3 years (3). Currently no consensus on follow-up schedules exists, outside of nonspecific close clinical follow-up.
TREATMENT:
The patient underwent a wide local excision with 3mm margins and had a intermediate linear closure. The excision specimen was sent for hematoxylin and eosin to check margins. This pathology was positive for residual neoplasm and a repeat wide local excision with 3mm margins was performed. The final pathology was clear and the patient healed without complication. Per guidelines in the literature the patient will return for close-follow up with yearly skin checks to monitor for recurrence.
REFERENCES:
Alves, J. V., Matos, D. M., Barreiros, H. F., & Bártolo, E. A. F. L. F. (2014). Variants of dermatofibroma – A histopathological study. Anais Brasileiros de Dermatologia, 89(3), 472-477. https://doi.org/10.1590/abd1806-4841.20142629
Fukamizu, H., Oku, T., Inoue, K., Matsumoto, K., Okayama, H., & Tagami, H. (1983). Atypical (“pseudosarcomatous”) cutaneous histiocytoma. Journal of Cutaneous Pathology, 10(5), 327-333. https://doi.org/10.1111/j.1600-0560.1983.tb00335.x
Calonje, E., Mentzel, T., Fletcher, C. D., & Path, M. R. (1994). Cellular benign fibrous histiocytoma. The American Journal of Surgical Pathology, 18(7), 668-676. https://doi.org/10.1097/00000478-199407000-00002
Elder, D. E., & Lever, W. (2015). Lever’s histopathology of the skin. Philadelphia: Wolters Kluwer.
Tsunoda, K., Oikawa, H., Maeda, F., Takahashi, K., & Akasaka, T. (2015). A case of cellular fibrous histiocytoma on the right elbow with repeated relapse within a short period. Case Reports in Dermatology, 7(1), 10-16. https://doi.org/10.1159/000371790
Macarenco, R. (2013). Faculty of 1000 evaluation for metastasizing “benign” cutaneous fibrous histiocytoma: A clinicopathologic analysis of 16 cases. F1000 – Post-publication peer review of the biomedical literature. https://doi.org/10.3410/f.717981109.793477863