CORRECT DIAGNOSIS:
Pemphigus Vegetans
DISCUSSION:
Pemphigus vegetans was first described by Neumann in the late 1800’s. The disease is characterized as a variant of pemphigus vulgaris (PV) and represents only 1-2% of all pemphigus patients. Pemphigus vegetans occurs in people of all ages but most prevalent in the fourth to fifth decades of life. The disease has a higher incidence in females.
Pemphigus vegetans is clinically characterized by vesicles and bullae which rupture leaving erosions. Vegetative plaques then develop on the eroded base giving rise to the distinct clinical picture of pemphigus vegetans. The classic sites of involvement are flexural surfaces, axillae and inguinal folds, although other sites can be involved. Mucosal findings including ulcerations and fissured tongue are frequently observed.
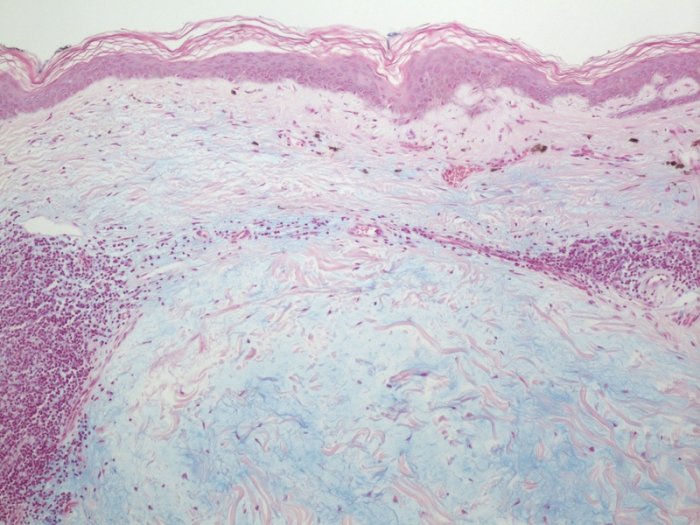
The etiology of pemphigus vegetans is unclear. There are postulations that pemphigus vegetans is PV with chronic colonization of bacteria or fungus leading to vegetations, although this has not been consistently observed. Pemphigus vegetans is known to have the same target antigens as PV, desmoglein 3 and sometimes desmoglein 1. This explains the early histopathological findings of suprabasal acantholysis in the epidermis secondary to anti-desmoglein 1 antibodies and suprabasal acantholysis in the mucosa secondary to anti-desmoglein 3 antibodies. Pemphigus vegetans shows papillomatous, verrucous or pseudoepitheliomatous hyperplasia which is not observed in PV. Eosinophilic intraepidermal microabcesses can also be seen. The dermis is edematous with an intense mixed inflammatory infiltrate. Immunofluorescence findings in pemphigus vegetans are indistinguishable from those of PV. Direct immunofluorescence reveals intercellular deposition of IgG and C3. Indirect immunofluorescence reveals circulating antiepithelial cell-surface IgG.
The differential diagnosis is limited due to the classic clinical presentation of pemphigus vegetans. Vegetative plaques can be seen in condyloma acuminata, condyloma lata, candidal intertrigo, halogenoderma, and paraneoplastic pemphigus. Hailey-Hailey disease could be included in the differential diagnosis due to the flexural involvement.
Treatment of pemphigus vegetans is similar to that of PV. Systemic glucocorticoids are first line therapy. Prednisone at 1.0 mg/kg/day is the preferred initial dosage. Response should be noted within the first two weeks of treatment. If no response is observed addition of other immunosuppressive agents may be necessary. Other systemic therapies include azathioprine, dapsone, cyclophosphamide, mycophenolate mofetil, cyclosporine, tetracyclines or etretinate. Topical treatments should not be overlooked. Using a corticosteroid soaked gauze to the intertriginous areas with antiseptics has proved to be efficacious.
TREATMENT:
Patient was initially given prednisone 40mg daily for two weeks. He was then started on clobetasol propionate 0.05% gel twice daily to mouth, clobetasol propionate 0.05% cream twice daily to skin lesions and tacrolimus solution swish and spit for oral lesions. Upon follow up, most lesions have resolved with residual post-inflammatory hyperpigmentation.
REFERENCES:
1. Mesquita C, Igreja A. Pyodermatitis-pyostomatitis vegetans: A differential diagnosis of pemphigus vegetans. An Bras Dermatol. 2012. 87:339.
2. Ruocco V, et al. Pemphigus vegetans of the folds (intertriginous areas). Clin. Dermatol. 2015. 33:471-476.
3. Zaraa, I, et al. Pemphigus vegetans: A clinical, histologic, immunopathological and prognostic study. J Eur Acad Dermatol Venereol. 2011. 25:1160-1167.