CORRECT DIAGNOSIS:
Hypopigmented Mycosis Fungoides
DISCUSSION:
Hypopigmented Mycosis Fungoides (MF) is a variant of early-stage cutaneous T-cell lymphoma, primarily affecting individuals with darker skin types, including those of African-American, South Asian, Middle Eastern, and Hispanic descent. This subtype often presents at an earlier age than conventional MF, most commonly affecting the pediatric population.
Clinically, hypopigmented MF is characterized by hypopigmented to achromic lesions that may manifest as patches or thin plaques, often accompanied by fine scaling. These lesions vary in size from small droplet-sized spots to larger plate-sized areas and are typically found on the trunk, buttocks, pelvic girdle, and lower limbs, often in areas with minimal sun exposure.
Patients with hypopigmented MF may experience varying degrees of itchiness, although local sensitivity is generally preserved. In some cases, patients may present with erythroderma and generalized lymphadenopathy. The lesions can exhibit atrophy and telangiectasia and may become more pronounced following sun exposure.
Diagnosing hypopigmented MF can be challenging, as its presentation can mimic other dermatological conditions such as atopic dermatitis, vitiligo, and pityriasis alba. To minimize delays in diagnosis, it is crucial to biopsy any suspicious skin lesions. Histological examination, along with electron microscopy, typically reveals a decreased number of melanosomes within epidermal keratinocytes, while melanin-producing melanocytes may display normal morphology. A deficiency in melanosomal transfer is commonly noted, particularly in cases of post-inflammatory hypomelanosis.
T-cell intracytoplasmic antigen 1 (TIA1) is a cytotoxic molecule that is constitutively expressed by CD8+ cytotoxic T cells, regardless of their activation state. In the context of hypopigmented Mycosis Fungoides (HMF), research indicates that malignant CD8+ lymphocytes typically exhibit TIA1 positivity. This characteristic distinguishes them from malignant CD8– lymphocytes, which are generally TIA1 negative. This differential expression of TIA1 may have implications for understanding the behavior and prognosis of malignant lymphocyte populations in HMF, highlighting the relevance of TIA1 as a potential biomarker in this condition.
Regulatory T cells (Tregs) are known to inhibit immune responses against tumors and are identified by the immunophenotype CD4+ CD25+ FOXP3+. In hypopigmented MF, there is a decreased ratio of FOXP3+/CD4+ and FOXP3+/CD25+ cells compared to conventional MF. This reduction in Tregs may influence the immune environment and response to malignancy in hypopigmented MF.
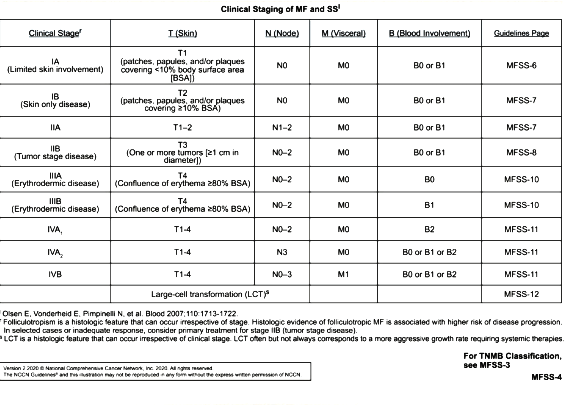
Diagnostic testing for hypopigmented MF includes skin biopsies (with serial biopsies sometimes necessary), immunophenotyping, and T-cell gene rearrangement analysis. Routine blood work, including a complete blood count (CBC) with differential, may also be performed, along with consideration of HTLV-1 serology and lymph node examinations. Depending on clinical manifestations, additional diagnostic tools such as CT imaging, chemistry panels, and bone marrow biopsies may be warranted for accurate staging.
TREATMENT:
Treatment for hypopigmented MF is tailored to the clinical stage at presentation. First-line therapies often include topical corticosteroids and narrowband ultraviolet B (NBUVB) phototherapy, both of which are generally safe and effective. Successful treatment typically results in repigmentation of hypopigmented lesions, and consultation with oncology specialists is advised to optimize management. Our patient opted for topical corticosteroid therapy.
CONCLUSION:
Hypopigmented MF is a distinct variant of cutaneous T-cell lymphoma that primarily affects individuals with darker skin tones, presenting significant diagnostic challenges due to its resemblance to other skin conditions. With an early age of average diagnosis, early recognition is crucial to initiate effective treatment and improve patient outcomes.
Given its variable presentation, the importance of biopsy in suspicious lesions cannot be overstated, as histological findings, such as a decreased number of melanosomes in epidermal keratinocytes, are key to differentiating hypopigmented MF from conditions like vitiligo and atopic dermatitis. Diagnostic workups may involve multiple tests, including T-cell gene rearrangement analysis and CT imaging, to accurately stage the disease and tailor treatment. The goal is often successful repigmentation, significantly impacting patients’ quality of life.
Given the complexities associated with hypopigmented MF, a multidisciplinary approach that includes both dermatology and oncology is essential. Regular follow-up care is vital to monitor for treatment response, manage potential side effects, and address any signs of disease progression. This comprehensive strategy aims to optimize outcomes and enhance the overall well-being of affected individuals.
REFERENCES:
Furlan, FC., & Sanches, JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. Anais brasileiros de dermatologia. 2013 Dec; 88(6): 954–960. [PMID 24474105]
Martínez Villarreal, A., Gantchev, J., Lagacé, F., Barolet, A., Sasseville, D., Ødum, N., Charli-Joseph, YV., Hernández Salazar, A., & Litvinov, IV. Hypopigmented Mycosis Fungoides: Loss of Pigmentation Reflects Antitumor Immune Response in Young Patients. Cancers. 2020 Jul; 12(8):2007. [PMID 32707930]
Alojail, HY., Alshehri, H., & Kaliyadan, F. Clinical Patterns and Treatment Response of Patients With Mycosis Fungoides a Retrospective Study. Cureus. 2022 Jan; 14(1), e21231. [PMID 35174031]