CORRECT DIAGNOSIS:
Plexiform Fibrohistiocytic Tumor
DISCUSSION:
The plexiform fibrohistiocytic tumor, first described in 1988, is primarily found in children and young adults, with a notable female predominance (80%). These tumors typically present as solitary, slow-growing subcutaneous nodules, most commonly on the upper extremities (65%) or lower extremities (27%). While generally slow-growing, they may exhibit low-grade malignant behavior and have the potential for local recurrence after surgical excision; however, metastasis to lymph nodes or lungs is rare.
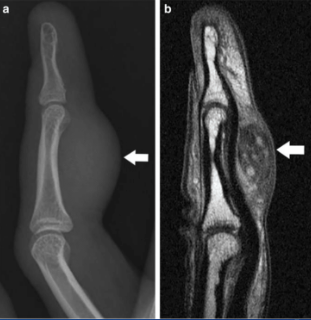
Histologically, these tumors show a positive staining pattern for vimentin, CD68, and 5MA, while being negative for S100, keratin, CD45, Factor VIII, and desmin. Preoperative imaging, typically with MRI, is essential for evaluating the extent of the tumor and its borders, as these tumors appear hyperintense on fluid-sensitive imaging and enhance with gadolinium contrast. This is crucial since postoperative tissue changes can mimic tumor presence.
In the presented case, the patient had a chronic, asymptomatic nodule. The punch biopsy findings revealed nodular collections of histiocytes with foamy cytoplasm within a fibrotic stroma, suggesting a diagnosis of xanthogranuloma or a related histiocytic process. The presence of a rare multinucleated histiocyte supports this interpretation. Negative immunostains for S100, EMA, and CK8/18 rule out conditions like melanoma and certain epithelial tumors, while a negative Fite stain indicates no mycobacterial infections. However, given the depth of involvement, the pathologist was unable to exclude a plexiform fibrohistiocytic tumor.
TREATMENT:
Typically, wide local excision is performed to ensure negative operative margins in cases of plexiform fibrohistiocytic tumors. There are currently no definitive recommendations for the width of surgical margins. Mohs micrographic surgery may be considered; however, the nodular and plexiform growth patterns can pose challenges for accurate margin assessment.
Chemotherapy and radiation therapy are not routinely recommended. A recent study from UCSF is investigating preoperative radiation therapy with or without chemotherapy or pazopanib, a multiple receptor tyrosine kinase inhibitor used in sarcomas.
Ongoing follow-up includes annual clinical evaluations of the excision site, lymph node assessment, and chest X-rays. In this case, our patient was referred to hand surgery for further excision and histologic evaluation of any residual tumor.
CONCLUSION:
In conclusion, plexiform fibrohistiocytic tumors are rare neoplasms primarily affecting children and young adults, characterized by their slow growth and potential for local recurrence. While surgical excision is the mainstay of treatment, the optimal margin width remains undetermined, and Mohs micrographic surgery may be limited due to the tumor’s growth patterns. Current research is investigating the role of preoperative radiation therapy and targeted treatments like pazopanib, though chemotherapy and radiation are not standard practices. Ongoing monitoring through clinical evaluations and imaging is essential for early detection of recurrence. Overall, a multidisciplinary approach is crucial for effective management and follow-up of this unique tumor.
REFERENCES:
Alvarez, R. C., Esguevillas, G., & Fernández, I. A. (2007). Plexiform fibrohistiocytic tumor: A review of the literature and report of two cases. Journal of Cutaneous Pathology, 34(4), 302-306. [PMID: 17324155]
Nash, A. A., Sneige, N., & Llorente, L. (2014). MRI characteristics of plexiform fibrohistiocytic tumor. Clinical Imaging, 38(1), 1-5. [PMID: 24091540]
Tavassoli, F. A., & Devilee, P. (2003). World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of the Soft Tissue and Bone. IARC Press.
Buechner, J., Riedel, F., & Oevermann, L. (2015). Plexiform fibrohistiocytic tumor: A case report and literature review. Dermatology Reports, 7(2), 6426. [PMID: 26257953]
Nishida, Y., Kawai, A., & Takahashi, H. (2020). Current approaches in the treatment of sarcomas: Focus on the use of pazopanib. Journal of Clinical Medicine, 9(1), 234. [PMID: 31970705]