CORRECT DIAGNOSIS:
Generalized Pustular Psoriasis (vom Zumbush)
DISCUSSION:
Generalized pustular psoriasis (GPP) is a rare but severe variant of psoriasis characterized by widespread, sterile pustules and systemic symptoms. It is primarily associated with mutations in the IL36RN gene, leading to a deficiency of the interleukin 36 receptor antagonist, also known as DITRA. This condition is more prevalent in middle-aged Asian and Hispanic adults and can present rapidly with erythematous pustules, often affecting flexural areas, the anogenital region, and nails. Accompanying systemic symptoms may include fever, malaise, leukocytosis, and hypoalbuminemia, with hypocalcemia posing a significant risk.
While the exact etiology of GPP remains unclear, several triggers have been identified, including infections, abrupt cessation of corticosteroids, pregnancy, and certain medications such as NSAIDs, lithium, and TNF-alpha inhibitors. Topical irritants can also provoke flares. Extracutaneous manifestations may include cholestasis, cholangitis, arthritis, and oral lesions, indicating the systemic nature of the disease.
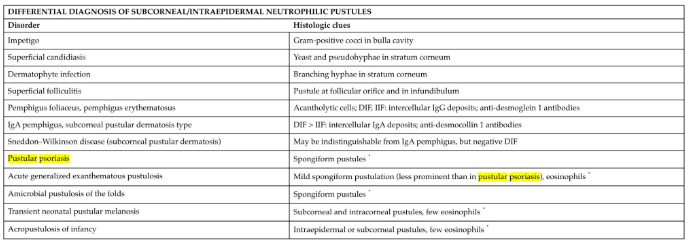
Diagnosis is primarily clinical, supported by histopathological findings. In the case of suspected GPP, histopathology may reveal characteristic pustules without evidence of infectious organisms, as seen with negative PAS, GMS, and Gram stains. Differential diagnoses, such as drug eruptions, erythema multiforme, Steven-Johnson syndrome, or toxic epidermal necrolysis, should be considered but are typically excluded based on specific histological features.
In this case, the histopathology report suggested that generalized pustular psoriasis was the most likely diagnosis. Differential diagnoses, such as a pustular drug eruption, were considered less probable. Notably, the characteristic changes associated with erythema multiforme, Steven-Johnson syndrome, or toxic epidermal necrolysis were absent. Additionally, staining techniques, including PAS, GMS, and Gram stains, returned negative for infectious organisms, further supporting the diagnosis of pustular psoriasis.
The prognosis for patients with generalized pustular psoriasis can vary widely depending on the severity of the disease and the presence of systemic complications. Prompt diagnosis and aggressive management are crucial to improving outcomes and preventing potentially life-threatening complications. Early intervention can significantly impact the overall quality of life and survival rates for affected individuals.
TREATMENT:
Management of generalized pustular psoriasis primarily involves a combination of nonbiologic and biologic therapies. Initial treatment may include nonbiologic agents such as corticosteroids, cyclosporine, acitretin, and methotrexate. For moderate to severe cases, systemic retinoids like acitretin, either alone or in combination with phototherapy, are often preferred due to their effectiveness. The joint guidelines from the American Academy of Dermatology and the National Psoriasis Foundation recommend several biologic therapies, including infliximab, adalimumab, ustekinumab, secukinumab, ixekizumab, and brodalumab, which have demonstrated efficacy as monotherapy. Notably, studies involving 292 patients have indicated that secukinumab and ixekizumab have the highest curative rates.
Recently, spesolimab, a selective monoclonal antibody targeting the interleukin-36 receptor, has received FDA approval for the treatment of generalized pustular psoriasis. In a 12-week, placebo-controlled trial with 53 adults, those treated with spesolimab exhibited significant improvements, with 54% showing no visible pustules after one week compared to just 6% in the placebo group. However, potential side effects of this treatment can include nausea, vomiting, headaches, pruritus, infusion site bruising, infections, and drug reaction with eosinophilia and systemic symptoms (DRESS).
For our patient, aggressive management was required upon hospitalization, including fluid and electrolyte replacement, intravenous steroids, and topical treatments with triamcinolone 0.1% ointment applied three times daily, along with wet wraps. She was started on acitretin at a dosage of 50 mg daily and infliximab infusions. Following the tapering of Solu-Medrol, she transitioned to an oral prednisone regimen of 60 mg daily. After discharge, she continued to follow up in our clinic and was referred to rheumatology. Currently, she is stable on Tremfya, weekly narrowband Ultraviolet B (NB-UVB) therapy, and 10 mg of methotrexate once a week with plans for tapering, and she has reported no new lesions.
CONCLUSION:
In summary, generalized pustular psoriasis is a rare and serious variant of psoriasis that requires immediate and aggressive treatment. It is characterized by widespread pustules and systemic symptoms, often linked to genetic mutations and various triggers. The management of generalized pustular psoriasis is complex and requires a multifaceted approach tailored to the individual patient’s needs. This rare and potentially life-threatening condition necessitates prompt hospitalization and aggressive treatment to stabilize the patient. In our case, the patient benefited from a combination of intravenous steroids, systemic retinoids, and biologic therapy, illustrating the importance of a comprehensive treatment plan. Regular follow-up and collaboration with specialists, such as rheumatologists, are crucial for monitoring the patient’s condition and adjusting the treatment regimen as needed. The successful outcome, with the patient remaining stable and free of new lesions, underscores the effectiveness of current therapeutic options, including oral and topical steroids, methotrexate, innovative biologic treatments like spesolimab, and established therapies like infliximab. Ultimately, a proactive and responsive management strategy can significantly improve the quality of life for patients suffering from this challenging dermatological disorder.
REFERENCES:
Bolognia, J. L., Schaffer, J. V., & Cerroni, L. (2018). Dermatology. Elsevier.
Papp, K. A., et al. (2021). Generalized pustular psoriasis: A review of the disease and its treatment. Journal of the American Academy of Dermatology, 85(5), 1095-1106. https://doi.org/10.1016/j.jaad.2021.06.019. [PMID: 34298810]
Alinaghi, F., et al. (2020). Generalized pustular psoriasis: A review of the literature. Dermatology Therapy, 33(5), e13953. https://doi.org/10.1111/dth.13953. [PMID: 32313647]
Guttman-Yassky, E., et al. (2021). New therapies for generalized pustular psoriasis. Nature Reviews Drug Discovery, 20(10), 749-750. https://doi.org/10.1038/d41573-021-00033-5. [PMID: 34338520]
Heymann, W. R. (2022). Treating generalized pustular psoriasis: The path forward. Journal of the American Academy of Dermatology, 86(6), 1234-1235. https://doi.org/10.1016/j.jaad.2021.10.006. [PMID: 34834490]
Abduelmula, A., Rankin, B. D., Sood, S., et al. (2023). Management of adult generalized pustular psoriasis using biologics: A systematic review. Journal of the American Academy of Dermatology, 89(2), 417-419. https://doi.org/10.1016/j.jaad.2023.04.032. [PMID: 37200322]
Papp, K. A., et al. (2021). Spesolimab: A novel treatment for generalized pustular psoriasis. British Journal of Dermatology, 185(6), 1244-1252. https://doi.org/10.1111/bjd.19898. [PMID: 33966521]
McCune, J. S., et al. (2022). An overview of systemic therapies for psoriasis. Expert Opinion on Biological Therapy, 22(6), 675-684. https://doi.org/10.1080/14712598.2022.2072020. [PMID: 35418375]
Kerdel, F. A., & Rojas, L. (2017). Generalized pustular psoriasis: A clinical review. American Journal of Clinical Dermatology, 18(3), 323-330. https://doi.org/10.1007/s40257-017-0280-4. [PMID: 28118606]
Elewski, B. E., Lebwohl, M. G., Anadkat, M. J., et al. (2023). Rapid and sustained improvements in generalized pustular psoriasis Physician Global Assessment scores with spesolimab for treatment of generalized pustular psoriasis flares in the randomized, placebo-controlled Effisayil 1 study. Journal of the American Academy of Dermatology, 89(1), 36-44. https://doi.org/10.1016/j.jaad.2023.01.008. [PMID: 37316591]