Presenter: Valeria González-Molina, MD, Thomas L Davis, MD, Rick Lin, DO
Dermatology Program: South Texas Dermatology Residency, HCA Healthcare Corpus Christi Medical Center – Bay Area Program
Program Director: Rick Lin, DO MPH FAOCD
Submitted on: June 12, 2024
CHIEF COMPLAINT: “I have dark patches on both sides of my chest“
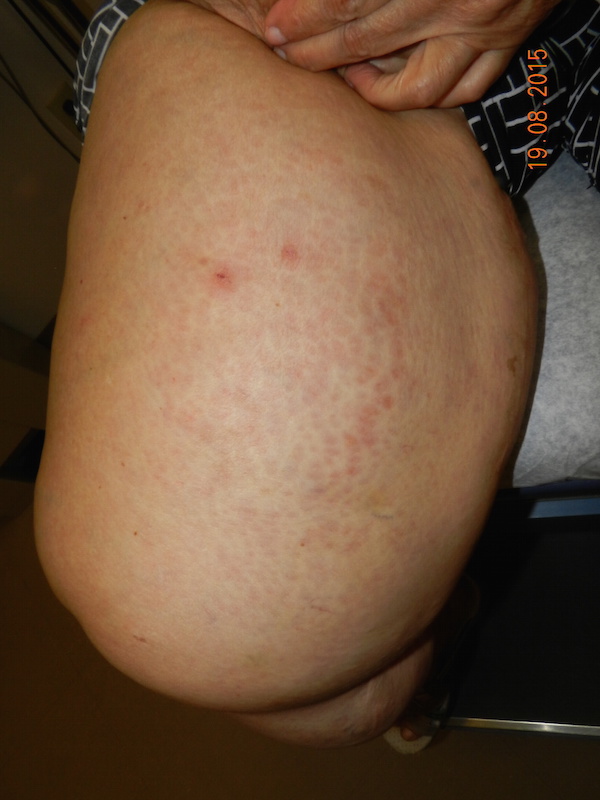
CLINICAL HISTORY: A 66-year-old Hispanic male presented to our clinic with a one-year history of mildly pruritic, purple to brown plaques located on both inframammary folds. The patient reported that the lesions first appeared one week after being hospitalized for a urinary tract infection complicated by sepsis. Initially, the lesions developed on the right inframammary fold and subsequently spread to the left side. He denies involvement of mucosal surfaces or nails. His medical history included diabetes, gout, hypertension, and dyslipidemia. He had a surgical history of a benign scrotal mass. He reported taking Novolog, Synjardy, allopurinol, lisinopril, metoprolol, and atorvastatin. The patient denied use of over-the-counter medications and reported no known drug allergies. He was a non-smoker, denied alcohol use, and was currently retired.
PHYSICAL EXAM:
Physical examination revealed a well-demarcated, violaceous-brown plaque with reticulated pattern on bilateral inframammary folds.
LABORATORY TESTS:
The patient’s laboratory results indicated a complete blood count (CBC) and comprehensive metabolic panel (CMP) within normal limits. Autoantibody screening revealed a negative antinuclear antibody (ANA) test. Thyroid function tests, including thyroid-stimulating hormone (TSH), triiodothyronine (T3), and thyroxine (T4), were all within normal ranges. Additionally, tests for tuberculosis and human immunodeficiency virus (HIV) returned negative results, and the hepatitis panel was also negative. Although the lipid panel showed elevated levels, it remains well-controlled given the patient’s medical history. The patient’s hemoglobin A1c level was recorded at 7.1%, indicating controlled diabetes, and urinalysis (U/A) results were within normal limits.
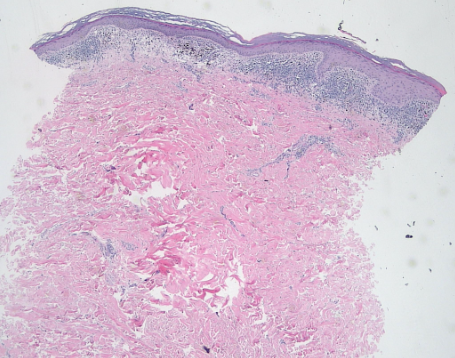
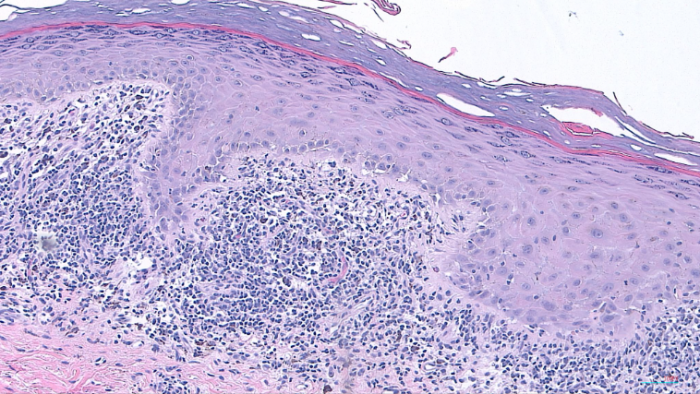
DERMATOHISTOPATHOLOGY:
The histopathological examination revealed several notable features consistent with a lichenoid tissue reaction. There was a band-like lichenoid infiltrate present in the papillary dermis, along with interface vacuolar degeneration affecting the basal cell layer of the epidermis. Additionally, pigmentary incontinence was observed in the upper dermis, indicative of melanin leakage. Hypergranulosis was noted, characterized by an increase in granules within the keratinocytes. The rete ridges exhibited a saw-tooth appearance, and Civatte bodies, which are apoptotic keratinocytes, were also identified.
DIFFERENTIAL DIAGNOSIS:
-
- Irritant Contact Dermatitis
- Inverse Psoriasis
- Fixed Drug Eruption
- Acanthosis Nigricans
- Candida Intertrigo
- Erythrasma
- Post-inflammatory Pigmentation
- Lichenoid Toxic Dermatitis
- Erythema Dischromicum Perstans
- Lichen Planus Pigmentosus-Inversus