CORRECT DIAGNOSIS:
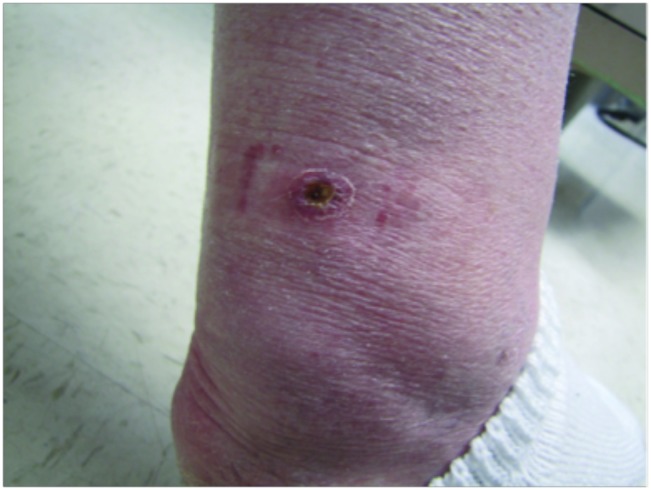
Pseudomonas Nail Infection
DISCUSSION:
Pseudomonas species are gram-negative, aerobic coccobacilli commonly found in various environments, including soil, water, plants, and animals. They are notable opportunistic pathogens that can cause infections in humans, particularly in vulnerable populations. Pseudomonas infections are frequently associated with exposure to moist environments, making certain occupational groups more susceptible.
Pseudomonas infections are especially prevalent among individuals working in occupations that involve prolonged exposure to water and chemicals, such as hairdressers, dishwashers, food handlers, and healthcare workers. These environments create ideal conditions for the bacteria to thrive, increasing the risk of colonization and infection. While such infections are rare in children, they can occur in immunocompromised individuals, including those with underlying health conditions or weakened immune systems. This susceptibility highlights the importance of understanding the risk factors associated with Pseudomonas infections in different populations.
Clinically, Pseudomonas nail infections typically manifest in areas of the nail plate that are exposed to onycholysis—a condition where the nail separates from the nail bed. One of the hallmark signs of a Pseudomonas infection is the development of greenish-black discoloration of the nail bed, primarily due to the production of the pigment pyocyanin. Patients often report pain and discomfort, along with potential nail fragility. In some cases, there may be associated inflammation or purulent discharge, which can further complicate the clinical picture.
Diagnosis of Pseudomonas nail infections involves a thorough clinical examination of the appearance of the nails and surrounding tissue, microbiological culture to confirm the presence of Pseudomonas species, and in certain cases, a biopsy to rule out alternative diagnoses.
TREATMENT:
Treatment for Pseudomonas nail infections typically begins with the application of topical gentamicin, using a 0.3% solution daily under the free edge of the nail. An alternative approach involves soaking the affected fingers in a solution of 0.1% polymyxin B and 1% acetic acid twice daily for one hour. The recommended duration for these treatments is approximately 1.4 months, with consistent topical applications generally required throughout this period. Our patient was started on gentamicin ointment with close follow-up.
If the topical treatments prove ineffective, oral ciprofloxacin may be prescribed at a dosage of 500 mg twice a day for 1-2 weeks. This comprehensive treatment strategy aims to effectively eliminate the infection while minimizing the risk of recurrence.
CONCLUSION:
Pseudomonas nail infections pose a notable risk, particularly in individuals with occupational exposure to moist environments and those who are immunocompromised. Understanding the epidemiology, clinical findings, and diagnostic strategies for these infections is critical for effective management and treatment. By recognizing the characteristic signs and implementing appropriate diagnostic measures, healthcare providers can mitigate the impact of Pseudomonas infections and ensure better outcomes for affected individuals. Awareness and education about prevention strategies, such as minimizing exposure to damp conditions, are also vital in reducing the risk of infection and recurrence.
REFERENCES:
Talarico, T., & Haffar, M. Pseudomonas aeruginosa Nail Infections: A Review. Journal of Clinical Microbiology. 2019; 57(2): e01240-18. [PMID 30536390]
Ramanathan, R., & Dhawan, A. Pseudomonas aeruginosa: A Potential Pathogen in Dermatology. Indian Journal of Dermatology. 2014; 59(5): 447-452. [PMID 25165609]
Wilkins, K., & Bhanusali, S. Nail Infections: Diagnosis and Management. American Family Physician. 2020; 102(6): 360-366. [PMID 32934116]
Dufresne, T., & Pottier, G. Clinical Presentation and Management of Pseudomonas Nail Infections. Clinical Microbiology Reviews. 2018; 31(1): e00053-17. [PMID 29237677]
Harris, D. J., & Enright, M. C. Opportunistic Infections in the Nail: Understanding Pseudomonas. Dermatology Clinics. 2016; 34(4): 581-590. [PMID 27476733]
Dawson, J., & Xu, C.Nail Disorders: Diagnosis and Treatment. Dermatologic Clinics. 2021; 39(3): 365-375. [PMID 33961545]