CORRECT DIAGNOSIS:
Lymphangioma Circumscriptum
DISCUSSION:
Lymphangioma circumscriptum, also known as microcystic lymphatic malformation, is characterized by ill-defined aggregates of small, abnormal lymphatic channels. This condition often arises from developmental anomalies during lymphatic vessel formation, which can result in disrupted lymphatic drainage. While the precise causes of these morphogenetic errors are not fully understood, factors such as genetic predispositions and environmental influences may play a role.
Typically present at birth, lymphangioma circumscriptum becomes more prominent during childhood, with most cases diagnosed in the early years. It primarily affects the proximal limbs and chest but can occur on any skin surface or within the oral cavity. Clinically, it appears as plaques with clusters of clear or hemorrhagic vesicles that vary in size, number, and color, and patients may experience swelling, bleeding, and lymph leakage from these vesicles. Complications can include erysipelas-like reactions, cellulitis, and other inflammatory responses.
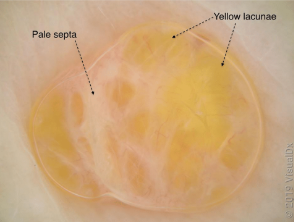
Dermoscopy reveals yellow, roundish areas called lacunae, surrounded by pale septa, which may also appear red or blue, aiding in diagnosis. This understanding is crucial for effective management and monitoring of the condition.
While a skin biopsy can confirm the diagnosis, lymphangioma circumscriptum is frequently diagnosed clinically due to its distinctive appearance. Ultrasonography can help assess the depth and extent of lesions before surgical intervention, while MRI and lymphangiography are valuable for identifying lymphatic cisterns in preparation for excision. These imaging techniques enhance the accuracy of diagnosis and guide effective management strategies.
TREATMENT:
Management of lymphangioma circumscriptum typically involves a “watch and wait” approach for asymptomatic lesions. In this case, the patient chose to closely monitor the lesions. Surgical intervention is usually considered for cosmetic reasons rather than immediate medical necessity, although recurrence rates can be as high as 23%. Symptomatic treatment options may include carbon dioxide laser therapy, long-pulsed Nd:YAG laser, electrosurgery, cryotherapy, superficial radiotherapy, compression, and sclerotherapy with hypertonic saline.
CONCLUSION:
Lymphangioma circumscriptum is a congenital lymphatic malformation that is primarily diagnosed based on its clinical presentation, with imaging studies like ultrasonography, MRI, and lymphangiography aiding in evaluation and treatment planning. While a skin biopsy can provide definitive confirmation, the characteristic appearance often suffices for diagnosis. Management typically involves monitoring for asymptomatic cases, with various treatment options available for symptomatic lesions. Understanding the condition’s complexities is essential for effective patient care and intervention.
REFERENCES:
Miceli A., Stewart KM. Lymphangioma. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Aug. PMID: 29261940.
Gomides, M., Costa, L., Berbert, A., & Janones, R. S. Cutaneous lymphangioma circumscriptum: The relevance of clinical, dermoscopic, radiological, and histological assessments. Clinical case reports. 2019 Apr; 7(4): 612–615. PMID 30997047
Blei, F., & Olivieri, A. (2016). Lymphatic malformations: A review of diagnosis and management. Pediatric Surgery International, 32(4), 339-346. https://doi.org/10.1007/s00383-016-3875-7
Lee, C. S., & Wysong, A. (2014). Lymphatic malformations: A review of the literature. Journal of Pediatric Surgery, 49(9), 1314-1320. https://doi.org/10.1016/j.jpedsurg.2014.04.021
Adigun, CG., Tan, B., Hocker, S., & Goldsmith, LA. Lymphangioma circumscriptum. VisualDx. 2020 Mar.