Presenter: Lawrence A. Schiffman, D.O.
Dermatology Program: St. John’s Episcopal Hospital, South Shore, Far Rockaway, NY
Program Director: Marvin Watsky, D.O.
Submitted on: May 15, 2008
CHIEF COMPLAINT: Rash on right arm
CLINICAL HISTORY: A 28-year-old man presents to the office for evaluation of a rash on his right arm. He reported an expanding rash on the right forearm during the previous 8 weeks. He complained of tenderness, itch, and yellow, pus-like discharge. He denied any antecedent trauma or insect bites. He also denied systemic symptoms such as fever, chills, myalgias or arthralgias. Three weeks earlier, he had seen his primary physician who had given him topical halobetasol 0.05% (Ultravate), oral prednisone, and ciprofloxacin. He was unsure of the dosage, but reported worsening of the condition, and stopped using the prescribed therapy. He stated that he was healthy and did not take any other medications. He had no known drug allergies. His family history was significant for Diabetes mellitus type II in his father. He drank alcohol socially and did not smoke. Interestingly, he worked as a sandblaster!
PHYSICAL EXAM:
The initial examination was documented as ‘an irregular, erythematous, annular patch with a raised border and overlying scale and crust’ located on the right medial forearm. The complete examination of the skin, oral mucosa, hair, and nails revealed early androgenetic alopecia. There was no cervical or axillary lymphadenopathy. No additional studies (ie. KOH, bacterial, fungal cultures) were performed and no image was obtained.
The patient was diagnosed with Tinea corporis and treated with oral ketoconazole tablets 200mg daily, and betamethasone 0.05%/clotrimazole 1% (Lotrisone) cream. He called three days later to report that “his infection was getting out of control” and that he was “very worried”. He was told to return to the office immediately.
Follow up examination of the right, dorsal forearm revealed a discrete, well-demarcated, 4.2 x 5.6cm erythematous, violaceous, ulcerating plaque with an irregular, serpiginous raised border. The lesion had associated blue-black, friable pustular areas. Further physical examination was non-contributory.


The patient was questioned further about his medical history and he revealed that he had been diagnosed with Ulcerative colitis three years earlier. This had required treatment with balsalazide (Colazal), mesalamine (Asacol), azathioprine (Imuran), and Prednisone as needed for a flare of symptoms. He explained that he went off his prior treatment regimen against the advice of his physician because he felt no symptoms of his disease.
LABORATORY TESTS: N/A
DERMATOHISTOPATHOLOGY:
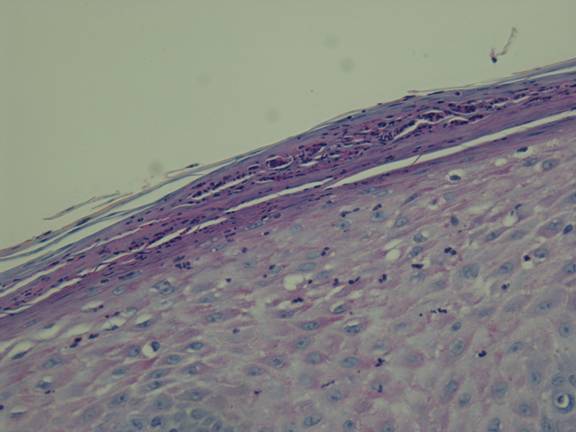
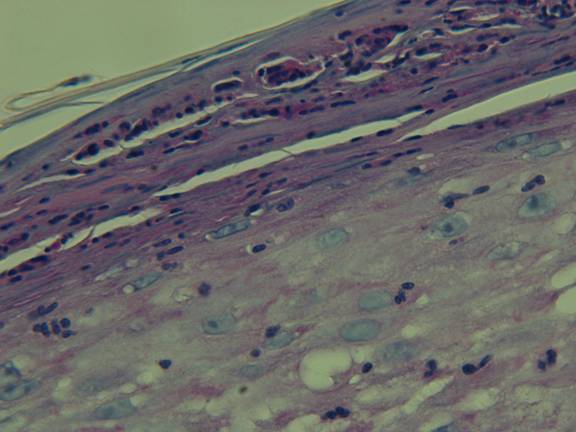
A 4mm punch biopsy specimen was obtained from the advancing edge of the lesion and it was sent for dermatohistopathology. A PAS stain was requested. No cultures were obtained. The epidermis exhibited parakeratosis and irregular acanthosis with spongiosis and exocytosis.
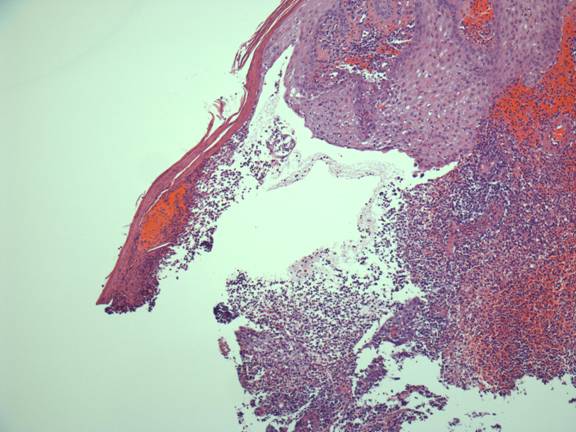
Within the dermis, there was a massive inflammatory infiltrate composed of lymphocytes, numerous sheets of neutrophils, histiocytes, and rare eosinophils. Hemorrhage was extensive.
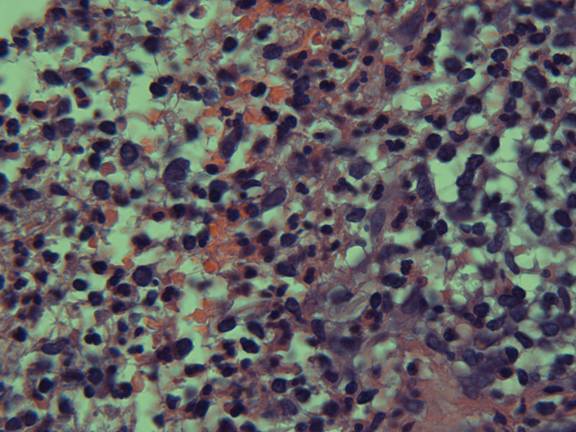
The PAS stain failed to reveal fungal elements. The findings were those of intense inflammation with ulceration. The changes could have been quite compatible with pyoderma gangrenosum or other forms of pyoderma. There was no evidence of dermatophyte infection or malignancy.
DIFFERENTIAL DIAGNOSIS:
1. Pyoderma gangrenosum
2. Insect/Spider bite reaction
3. Bullous Tinea corporis
4. Vasculitis
5. Aggressive neoplasm




