Presenter: Betsy Leveritt, DO
Dermatology Program: Wellington Regional Medical Center
Program Director: Brad Glick, DO
Submitted on: August 14, 2010
CHIEF COMPLAINT: Diffuse painful plaques
CLINICAL HISTORY: A 52-year-old Caucasian male with a past medical history of liver cirrhosis, subsequent hepatorenal syndrome, and end-stage renal disease (ESRD) on hemodialysis (HD), presented with a several month histories of numerous painful, erythematous-violaceous plaques across the abdomen and bilateral thighs and upper extremities, accompanied by necrotic erosions of the lower extremities. A review of systems revealed low-grade fevers with occasional chills, night sweats, and a significant weight loss of at least 13.6 kg over the preceding 3-4 months. During prior hospital admission, the patient manifested these same skin lesions, and was given a 3-month course of intravenous antibiotics for a biopsy-proven Actinomyces infection. He also recalled being given Heparin during that same hospital stay.
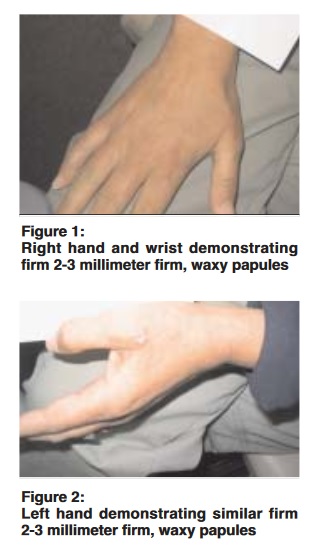
PHYSICAL EXAM:
Physical examination revealed a cachectic appearing male. Erythematous-violaceous, annular and reticulated, infiltrative appearing plaques were noted across the abdomen, inner thighs, and upper extremities. 12-16 cm erosions with necrotic centers, jagged edges, and pink, slightly rolled borders with a lack of undermining were also seen on both lower extremities. The pedal and popliteal pulses were 1-2+/4 bilaterally.


LABORATORY TESTS:
Pertinent laboratory studies revealed an elevated blood urea nitrogen (BUN) 45 mg/dL and creatinine 4.3 mg/dL, with a normal calcium 8.8 mg/dL, ionized calcium 1.3 mmol/L, and parathyroid hormone intact (PTHI) 15.6 pg/mL. Phosphorous was slightly elevated at 5.3 mg/dL. A calcium-phosphorous product was normal at 46.64 mg/dL. Albumin was decreased at 1.1 mg/dL, and alkaline phosphatase was elevated at 286 units/L. A heparin pf4 antibody was critically high. Furthermore, the lupus antiphospholipid antibody was positive at greater than 8 seconds, accompanied by an elevated APTT 1.5 hour at 46 seconds and an APTT 1:1 saline at 57 seconds. LA 1 (DRVVT) and LA2 (DRVVT) were normal. The remainder of the lupus anticoagulant panel was also negative. IgG was elevated at 1730 mg/dL, with a normal IgM level. A decrease in protein C antigen at 43% was also noted. However, protein S, both free and total, were normal at 76% and 69%, respectively. ANA, rheumatoid factor, as well as cryoglobulins were all negative. The patient was also anemic, with a hemoglobin (Hgb) 10.5 g/dL and hematocrit (HCT) 32.3%, as well as thrombocytopenic with a platelet (PLT) count of 107 K/mcl. HIV, Hepatitis B, and Hepatitis C serologies were negative. Tissue culture and smears for aerobic and anaerobic bacteria, fungi, and acid fast bacilli (AFB) were also negative. Paracenteses were negative for infection and malignancy.
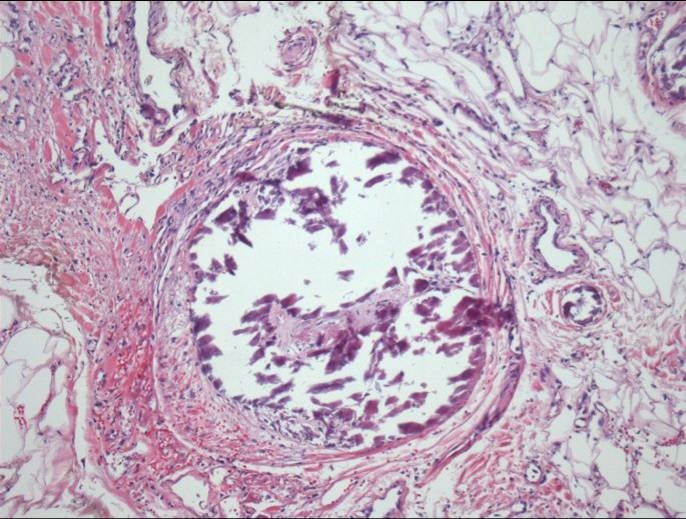
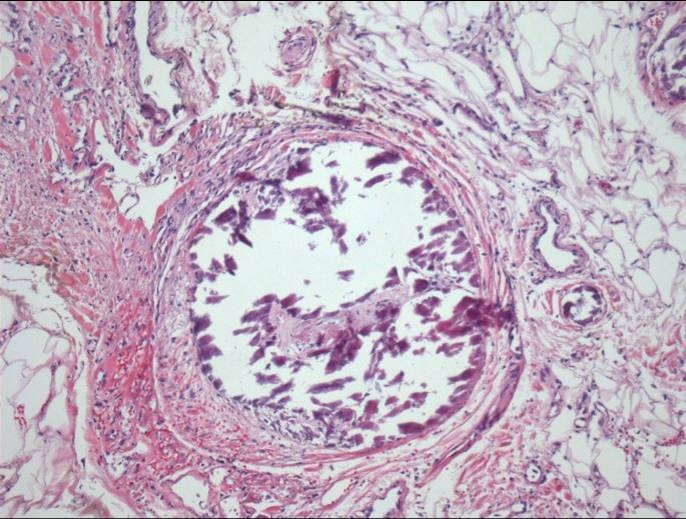
DERMATOHISTOPATHOLOGY:
Histopathology revealed intravascular calcification of small and medium-sized blood vessels associated with focal thrombosis, with adjacent secondary fibrosis and reactive neutrophilic infiltrate (Figure 3). A Von Kossa stain also showed intravascular calcium deposition. No primary vasculitis was evident. PAS and Fite stains were negative for micro-organisms. Direct immunofluorescence was also negative for vascular deposition of immunoreactants.
DIFFERENTIAL DIAGNOSIS:
1. Medium vessel vasculitis ( i.e. polyarteritis nodosa)
2. Inflammatory/ connective tissue disorder (nephrogenic fibrosing dermopathy , lupus panniculitis, pyoderma gangrenosum, and erythema nodosum)
3. Infectious etiology (cellulitis, septic emboli, ecthyma gangrenosum, necrotizing fasciitis, mucormycosis, aspergillosis)
4. Hypercoaguable-occlusive states (i.e. underlying malignancy, antiphospholipid antibody syndrome, protein C or S deficiency, factor V Leiden deficiency hyperhomocysteinemia)
5. Heparin or warfarin-induced skin necrosis