Presenter: Courtney N. Bernett, DO, Logan Kolb, DO, and Shawn Schmieder, DO
Dermatology Program: Orange Park Medical Center/Park Avenue Dermatology
Program Director: Karthik Krishnamurthy, DO
Submitted on: December 5, 2017
CHIEF COMPLAINT: ¨Itchy sore blisters on forearms”
CLINICAL HISTORY: A 62-year old male was referred to the dermatology clinic by his primary care physician (PCP) for a blistering rash on his arms. Three months prior to his presentation, he started to develop severe pruritus on his bilateral forearms. Shortly after the pruritus started, he developed large, blood-tinged blisters on his forearms. These blisters would rupture, leak fluid, and dry up. The patient saw his PCP for his blisters and they suspected a drug reaction to Lisinopril which had recently been started prior to his rash. His lisinopril was discontinued and changed to metoprolol with no change in his blisters. No topical treatments were attempted at that time. The patient has a past medical history of diabetes mellitus type 2, hypertension, and gastroesophageal reflux disease. He denied a personal or family history of hepatitis B or C, autoimmune disease, irritable bowel disease, or a history of recent travel. He has no known allergies, and his medications include metformin 500mg QD, metoprolol succinate 50mg QD, and omeprazole 40mg QD.
PHYSICAL EXAM:
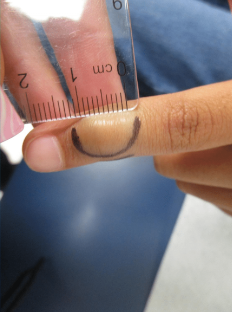
Well-appearing 62-year old male with multiple coalescing erosions with crusts on an erythematous base on the bilateral forearms.
LABORATORY TESTS: N/A
DERMATOHISTOPATHOLOGY:
The patient’s histopathology returned as the following:
Left forearm : Epidermal acanthosis with mild dermal fibrosis and a mixed dermal infiltrate with eosinophils
Comment: The histological features are not specific. There is no evidence of blister formation. The dermal infiltrate is mixed lymphocytes, plasma cells, and eosinophils. Focally, eosinophils are present at the dermal-epidermal junction which suggests the possibility of urticarial phase bullous pemphigoid, however the DIF results below are consistent with epidermolysis bullosa acquisita (EBA). EBA can show very similar histological findings to bullous pemphigoid. Clinical correlation recommended.
Left forearm: DIF- Positive
Comment: There is thick meshy linear IgG and much weaker IgA deposition along the dermal side of the split epidermal basement membrane zone. There is no C3, IgM, C5b-C9, or fibrinogen deposition observed in the specimen. These immunofindings are virtually diagnostic for EBA. Clinical and histological correlation is recommended. Multiple immunoreactant dilutions and sections were performed.
The classic histopathological findings for EBA include subepidermal cleavage without acantholysis on H+E.
In BP-like or mucous membrane pemphigoid-like variants, 劤 there is a variable inflammatory infiltrate in the dermis with neutrophils, eosinophils, or lymphocytes. On DIF, IgG is frequently seen in a continuous, broad, linear pattern around the basement membrane zone. Occasionally deposits of C3, IgA, or IgM may be found as well. In salt-split skin, immune deposits are found on the dermal side of the specimen. Immune electron microscopy is considered the ¨gold standard〃 of diagnosing EBA if none of the other methods are able definitively provide a diagnosis.
DIFFERENTIAL DIAGNOSIS:
1. Bullous pemphigoid
2. Pemphigus vulgaris
3. Bullous drug eruption
4. PCT
5. Pseudoporphyria