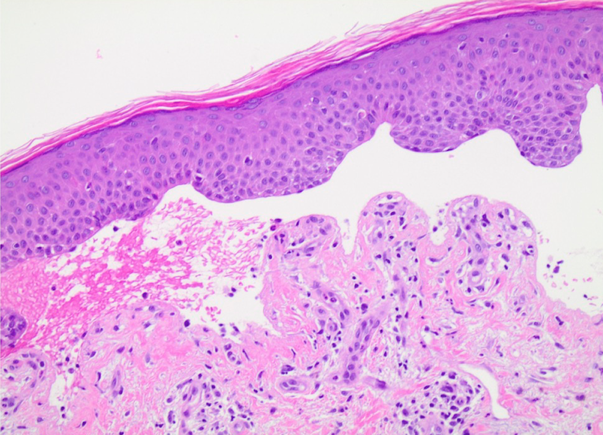
Pruritic blistering eruption on the forearms of a 60 year old male
Presenter: Courtney N. Bernett, DO, Logan Kolb, DO, and Shawn Schmieder, DO
Dermatology Program: Orange Park Medical Center/Park Avenue Dermatology
CHIEF COMPLAINT: ¨Itchy sore blisters on forearms”
CLINICAL HISTORY: A 62-year old male was referred to the dermatology clinic by his primary care physician (PCP) for a blistering rash on his arms. Three months prior to his presentation, he started to develop severe pruritus on his bilateral forearms. Shortly after the pruritus started, he developed large, blood-tinged blisters on his forearms. These blisters would rupture, leak fluid, and dry up. The patient saw his PCP for his blisters and they suspected a drug reaction to Lisinopril which had recently been started prior to his rash. His lisinopril was discontinued and changed to metoprolol with no change in his blisters. No topical treatments were attempted at that time. The patient has a past medical history of diabetes mellitus type 2, hypertension, and gastroesophageal reflux disease. He denied a personal or family history of hepatitis B or C, autoimmune disease, irritable bowel disease, or a history of recent travel. He has no known allergies, and his medications include metformin 500mg QD, metoprolol succinate 50mg QD, and omeprazole 40mg QD.